Menopause: A Pain in the Butt
Gluteal tendinopathy in post menopausal women
It might not just be the hot flashes keeping you up at night. Do you struggle to find a comfortable position while falling asleep, tossing from lying on one side to the other? Does the side of your hip ache or throb no matter which side you choose?
Gluteal tendinopathy is a common cause of lateral hip pain. Women, especially over the age of 40 years old, are about 2.4 to 4 times as likely to suffer from this condition compared to men1. The shape of the female pelvis is one possible contributor1, however, more recent studies have looked at the effect of hormones, specifically estrogen, on tendon health2. Post menopausal women have decreased levels of estrogen, which may be why gluteal tendinopathy is more prevalent in this population, affecting 1 in 4 women over the age of 503.
What is gluteal tendinopathy?

Gluteal tendinopathy affects the tendons that connect the muscles in your butt, usually the gluteus medius and minimus that attach to the side of your hip.
It is often caused by a combination of increased tensile and compressive loading. For example, this may happen if your hip drops when you walk or run and causes your leg to move towards your body’s midline. This action stretches the gluteal tendons over a bony bump on the outside of your hip called the greater trochanter.
If repeated often enough, this combination of tension and compression can lead to an irritated tendon with decreased tolerance to either load. For instance, body positions such as sitting with your legs crossed may now result in pain from the compression of the gluteal tendon stretching over the top of the thigh bone (femur).
Symptoms of gluteal tendinopathy
In addition to experiencing pain in the hip, this pain may extend down the outside of your leg to your knee or lower leg. Some people also experience pain in the lower back, groin, or gluteal.
The pain may feel worse when you:
- walk up/down a hill or stairs
- run
- lie on your side
- sit or stand cross legged
- stand on one leg
- move from a sitting to standing position
Learn more about gluteal tendinopathy and how to distinguish it from bursitis here
How to get rid of this pain in the butt?
Education
Education has been shown to play an important role in settling down an aggravated gluteal tendon. Pay attention to your body position and how you sit, stand, walk, run, or sleep. Below are some examples of positions that can cause increased compression of the tendon – avoid these!

Sleep positions can also be modified to help reduce compression of the tendon as shown below.

Exercise
Exercise is also an important component to manage gluteal tendinopathy, just like in any other tendinopathy1, 2, 3, 4. Because tendons connect your muscles to your bones, using your muscles helps to remodel injured tendons.
The LEAP and the GLoBE research studies showed that tendon-specific exercise improved symptoms3,4. Dr. Alison Grimaldi has some great infographics on her website that summarize the exercises used (see below)7.
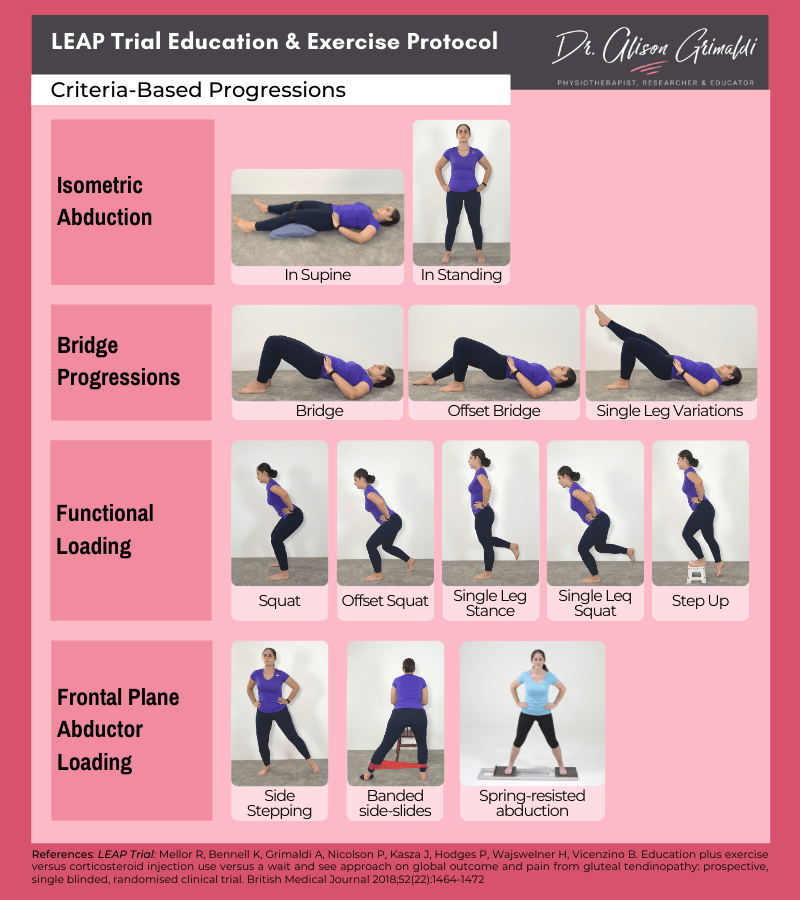
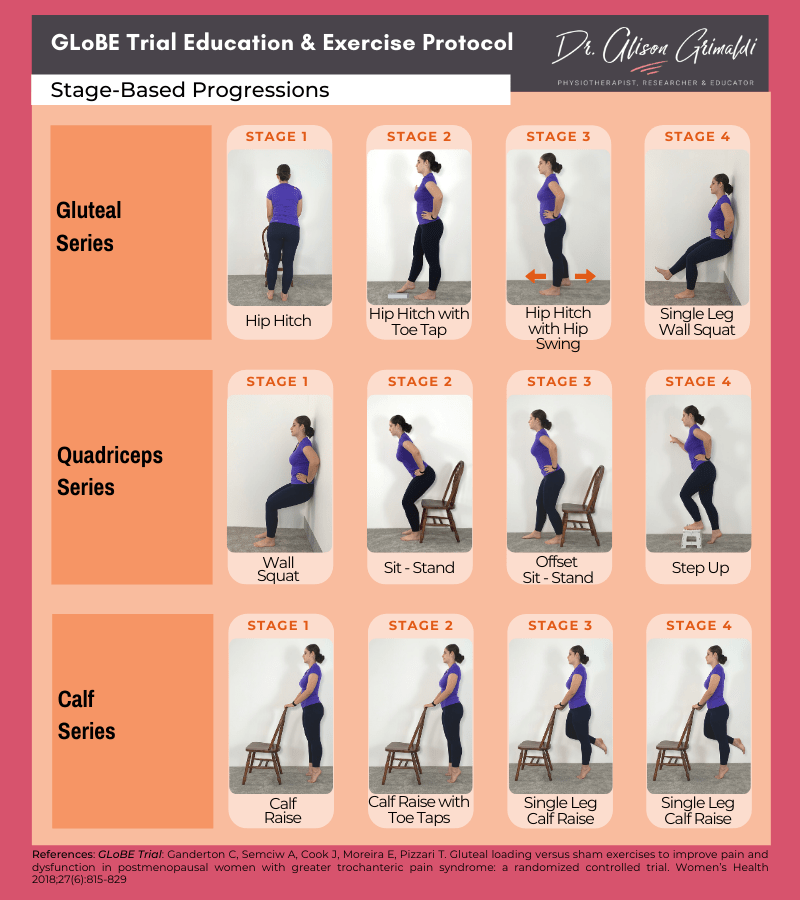
Although these offer some good suggestions, it is often beneficial to see a physiotherapist to get an individualized exercise program tailored to your current abilities.
A physiotherapist can also assess if how you walk or run may be contributing to your hip pain. People with gluteal tendinopathy often have higher hip adduction moments with walking5. In other words, their thigh bone moves more towards the body’s midline, causing more compression on the outside of the hip.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) combined with exercise has shown some promising results in a recent study by Cowan et al. (2022). In this study, supplemental estrogen was delivered topically in the form of a transdermal cream.
When the cream was used in combination with exercise, postmenopausal women that were of a healthy weight (with a Body Mass Index (BMI) less that 25) reported improvements in pain and symptoms. However, the cream did not appear to provide any additional benefit to women that were overweight (BMI 25 or greater). For women that fall into this category, supplemental hormones delivered in another way, for example, under the tongue (sublingual) may be of benefit.
Passive Treatment
Passive treatments such as shockwave therapy and corticosteroid injections may be considered if you are struggling to improve after several weeks of education and exercise. Although, many lower limb tendon rehabilitation programs recommend 6 to 12 months of exercise – so don’t give up too early and stick with it!
In fact, the LEAP trial showed that although corticosteroid injections can provide some short-term relief, education and exercise showed greater improvements in the longer-term at 8 weeks and 1 year3.
A recent study by Ramon et al. in 2020 found promising results when comparing 3 sessions over 3 weeks of shockwave vs. sham shockwave. Patients that received shockwave therapy reported experiencing less pain and improved function compared to those that received the sham treatment.
Shockwave therapy also known as Extracorporeal Shockwave Therapy (ESWT) delivers pressurized air waves to injured tissue

It’s important to keep in mind that the participants included in this study had hip pain lasting greater than 3 months and were excluded if they had other co-existing findings, such as calcification or persistent low back pain, which can often occur with gluteal tendinopathy6.
Overall the evidence supports education and exercise as a first line of treatment for gluteal tendinopathy. If after 3 months of consistent exercise and load modification you are still experiencing symptoms that are interfering with your life, you may want to consider adding passive treatments such as hormone replacement therapy and/or shockwave. Corticosteroid injections may play a role in helping those whose symptoms are so irritable that they need some short-term relief in order to complete an exercise program.
Contributing Expert

Alison Walford, Physiotherapist and pelvic health specialist at Banff Sport Medicine.