Trail Running & ITB Pain
It’s getting to that time of year again in the Rockies.
As the snow starts melting trail runners and hikers alike start to venture higher up into the alpine on foot.
Although many may have spent the winter ski touring or running the trails closer to valley bottom, the longer pounding descents on feet are a different type of load or stress on the body.
It’s not uncommon to get our first batch of iliotibial band (ITB) related knee pain complaints at the clinic with the change in seasons.
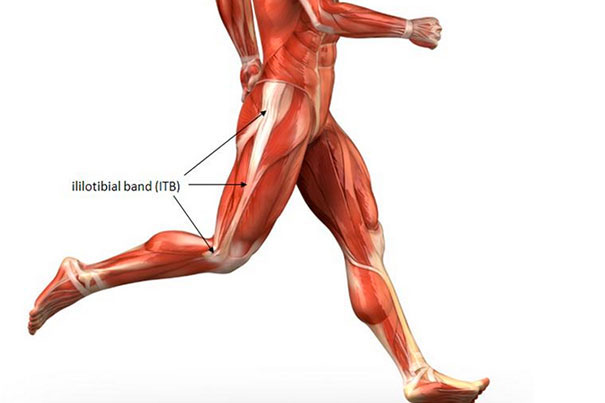
What is the ITB?
Contrary to what some people may think, the ITB is not a muscle, which is why they might have a hard time stretching it. The ITB is essentially a thickening in the fascia that envelops our quads.
Why can the ITB be so painful?
Between the ITB and the lateral femur at the knee there is fat tissue with lots of nerve endings.
When your knee bends to about 30 degrees there is maximum tension on the ITB, which can cause compression of this sensitive fat tissue.
Normally the brain does not interpret this as pain, however if you have exceeded the structure’s load capacity it will certainly tell you.
So there is a physiological reason why that sharp pain on the outside of your knee makes you want to walk like a pirate with a peg leg!
What are some risk factors for developing ITB pain?
#1. LOAD
ITB pain is an overuse injury, as most running injuries are. In a study by Hespanhol et al. (2016)1 on running-related injuries in Dutch trail runners, they reported that 75.2% were overuse injuries.
Furthermore, in 2021 Viljoen et al. published a study entitled “One in four trail running race entrants sustained an injury in the 12 months training preceding the 2019 SkyRun race”2. They found that 26.5% of all injuries reported were related to the knee, which was the highest incidence for one body part.
While running on flat ground, the quadricep muscle forces are 4 to 6 times your body weight depending on speed (Dorn et al., 2012)3. This number is likely higher while running downhill. The tensor fascia latae (TFL, a muscle that attaches to the ITB) and quads are both working hard eccentrically while running downhill, putting more load through the ITB.
#2. GAIT MECHANICS
Overstriding:
This is when your foot lands significantly in front of your centre of mass (CoM). The closer your CoM is to being above your landing foot, or in other words the more vertical your tibia (shin bone) on landing, the less stress put on your knee and hip.

Crossover:
Watch out for this one on narrower trails where your foot may often cross the midline of your body. Another sign of crossover gait may be if you often find mud on the inside of your calves after a trail run from your shoe hitting the other leg. This type of gait with more hip adduction can lengthen the ITB and put more pressure by it’s insertion.
Hip Drop:
You can often see this during mid-stance. If you are directly behind the person running you may notice their pelvis is not level. This again leads to more hip adduction which can cause more ITB compression.

What can you do to prevent ITB pain?
#1. I know how exciting it can be to finally have some traction under your feet running on dirt again, but the most common mistake is progressing load too quickly. As the snow melts this could mean accumulating elevation or increasing speed too rapidly, or both. You may not realize it right away either, because the injury may only peak about 3 weeks after the training error was made4.
#2. One of the easier and most effective ways to alter gait mechanics is to increase your cadence or the number of steps you take in one minute. Although 180 steps/minute is a frequently used target, even increasing your cadence by 5-10% has been shown to decrease patello-femoral loads by 15-20%, decrease peak hip adduction by 3-4 degrees, and reduce vertical ground reaction force (GRF) load rates by 18-22%4.
#3. Strength Training. Lastly I’ve included some strength exercises below to help load the ITB and to promote proximal control of the lower limb with hip and core strength. This may be done more frequently (eg 5x/week) if you are injured and not able to run. As you start a graded return to run or if you are already running and looking at prevention, this 20-30min strength routine can be done 2-3x/week. Note – some of these exercises are quite challenging. It is recommended to visit a physiotherapist to have a program tailored to your needs.
Modified Thomas
Split Squats
Side Plank with Hip Abduction
Front Plank with Donkey Kicks
Copenhagen Adduction
Single Leg Sit to Stand
Plyometric Rebounding Drill
Download a PDF version of this article
Contributing Expert

Alison Walford, Physiotherapist and passionate runner.
References
- Junior, L. C. H., Van Mechelen, W., & Verhagen, E. (2017). Health and economic burden of running-related injuries in Dutch trailrunners: a prospective cohort study. Sports Medicine, 47(2), 367-377.
- Viljoen, C. T., van Rensburg, D. C. C. J., van Rensburg, A. J., Booysen, E., Chauke, S., Coetzee, P., … & Cronje, T. (2021). One in four trail running race entrants sustained an injury in the 12 months training preceding the 2019 SkyRun race. Physical Therapy in Sport, 47, 120-126.
- Dorn, T. W., Schache, A. G., & Pandy, M. G. (2012). Muscular strategy shift in human running: dependence of running speed on hip and ankle muscle performance. Journal of Experimental Biology, 215(11), 1944-1956.
- Willy, Richard. (Physio Network). (2020). Restoring load capacity in the injured runner . https://www.physio-network.com/masterclass/restoring-load-capacity-in-the-injured-runner/
- Boren, K., Conrey, C., Le Coguic, J., Paprocki, L., Voight, M., & Robinson, T. K. (2011). Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. International journal of sports physical therapy, 6(3), 206.






