Hip Osteoarthritis: The Basics
Osteoarthritis is becoming increasingly common with more than 4.4 million people in Canada living with osteoarthritis; with hip osteoarthritis affecting approximately 3% to 8% of the general population.
If you have osteoarthritis, know that you are not alone. With the appropriate care, many people live meaningful, productive, and pain free lives despite this diagnosis.
Hip anatomy
The hip joint connects the thigh bone (femur) to the pelvis. This connection occurs between the head of the femur, which is shaped like a ball and the acetabulum of the pelvis, which is shaped like a cup. The acetabulum is a cup-like depression on the pelvis. It is found on either side of the lower pelvis and faces away from the body. The cup is deepened by a cartilage rim – called the labrum which helps with load distribution and stability in the hip.
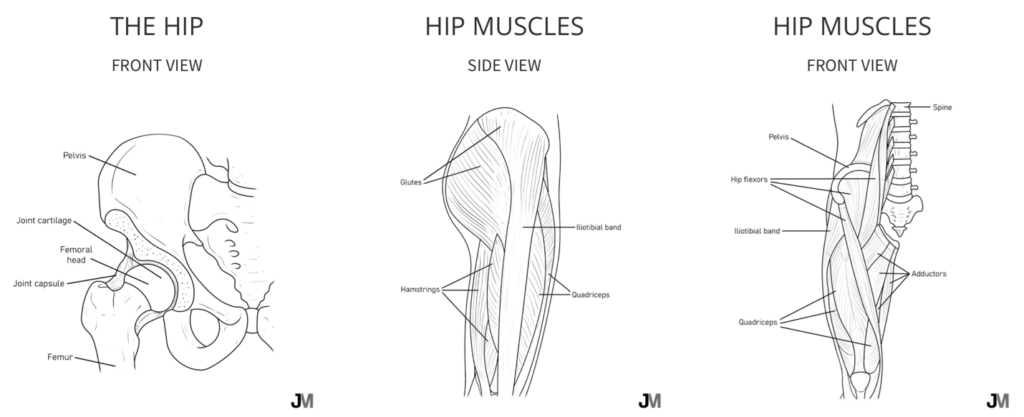
The head of the femur and acetabulum are covered in smooth articular cartilage, allowing the hip joint to move freely and smoothly. Articular cartilage is thicker at the places of weight bearing providing a low friction environment and cushion.
The hip joint is surrounded by a thick joint capsule and several ligaments. They help provide stability to the joint. The joint capsule releases synovial fluid which helps to lubricate the joint surfaces.
Finally, muscles from the trunk and thigh cross the hip joint providing movement and stability.
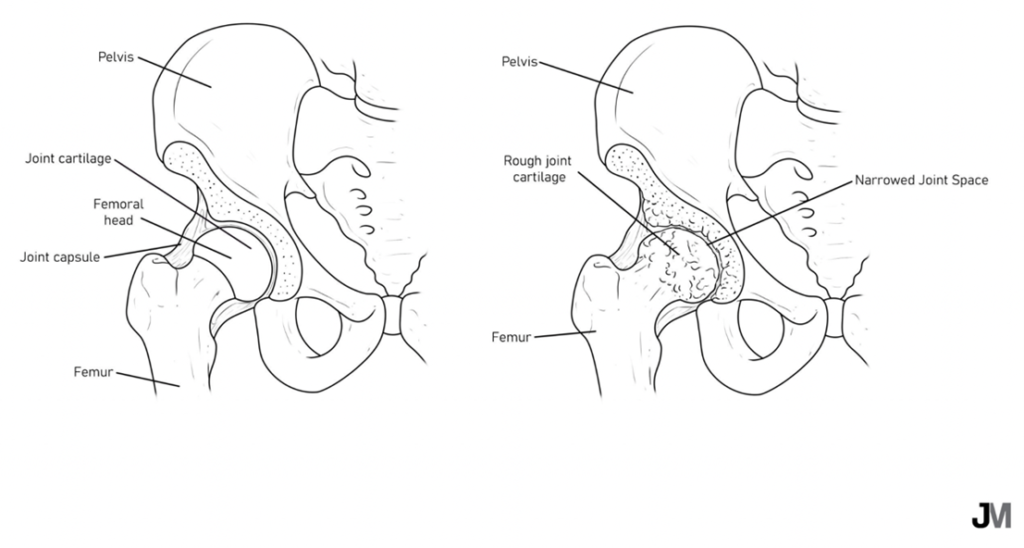
Hip osteoarthritis
Osteoarthritis of the hip involves changes to all the tissues in the joint, including cartilage, joint fluid, and bone. These changes can sometimes (but not always) lead to pain, stiffness, and decreased mobility. While these joint changes aren’t necessarily reversible, with the right treatment and lifestyle changes, many people are able to take control of their symptoms and significantly improve their quality of life.
What are the symptoms of hip osteoarthritis?
- Hip pain
- Hip swelling
- Sensations of stiffness in the hip joint
- Decreased range of motion in the hip joint
- Sensation or audible grinding/clicking/a “noisy” joint
- Decreased function that limits your ability to participate in daily activities
Does hip imaging tell me how much pain I will have?
You may be surprised to know that when it comes to hip osteoarthritis, we can’t look at an x-ray and know how much pain you will have or if you are going to have pain at all.
Sometimes a person will have severe pain but very minimal changes to their hip on their x-ray.
In other cases, someone will have significant changes on their x-ray but have no hip pain whatsoever.
The key here is that, in many cases, you can improve your pain, symptoms, and quality of life without changing how your hip looks on an x-ray.
How is hip osteoarthritis diagnosed?
Hip osteoarthritis is typically diagnosed by your healthcare provider by taking a detailed clinical history (i.e., asking you a variety of questions), performing a physical exam (i.e. feeling how your hip moves and watching you move), and by getting weightbearing x-rays of your hip.
Should I get an MRI?
Research has shown that relatively inexpensive x-rays provide enough detailed information for doctors to confirm the diagnosis of hip osteoarthritis, determine its severity, and make appropriate treatment recommendations.
Believe it or not, rarely do more expensive MRIs provide any additional information to manage your osteoarthritis.
Why did I develop osteoarthritis?
Osteoarthritis can develop because of several contributing factors.
These are some of the most common reasons individuals develop osteoarthritis:
- Sex (females are more likely to develop osteoarthritis than males)
- Increased age
- Past injury or surgery to the hip joint
- Substantial weight gain or obesity
- Joint alignment
- Genetics
- Occupation
- Diet
- Movement and physical activity
Managing Hip Osteoarthritis
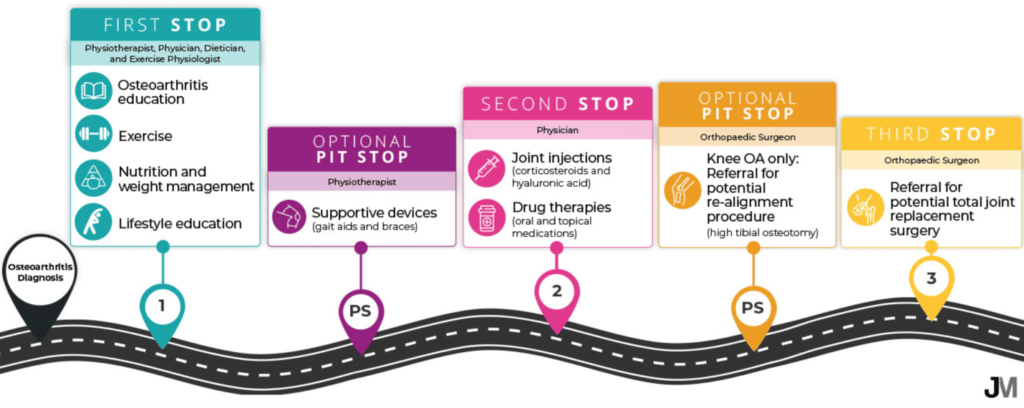
There are many options to begin to treat your osteoarthritis and optimize your joint heath, but it is important to understand that not all options are created equally.
Some treatments are proven to be more effective and worthwhile than others, and some options are recommended to be explored first before others are trialed.
Think of managing your hip osteoarthritis as a personal lifelong journey. The individual journey may look quite different for each person, but there is an ideal pathway to optimize your joint health.
Patients should first receive osteoarthritis education, exercise therapy, appropriate diet and weight loss if needed, and lifestyle education.
Additional use of supportive devices (gait aids, knee braces, etc.) may be beneficial. When these strategies no longer offer acceptable pain relief, drug therapies (painkillers and non-steroidal anti-inflammatory drugs) are considered the next step.
Lastly, joint injections may be recommended to you by your healthcare professional.
— Learn more about joint injections done at the Banff Sport Medicine Clinic —
Expert Contributor

Kristen Barton, MD, PhD, MSc, BSc (Hons), CSEP-CEP
Orthopaedic Surgery Resident, Western University
Adjunct Research Professor, Faculty of Health Sciences, Western University
Adjunct Assistant Professor, Faculty of Kinesiology, University of Calgary
Founder, Joint Management






