Understanding Multidirectional Shoulder Instability
The shoulder is the most mobile joint in the human body.
While the shoulder’s remarkable flexibility allows for a wide range of motion, excessive movement can also lead to pain and instability.
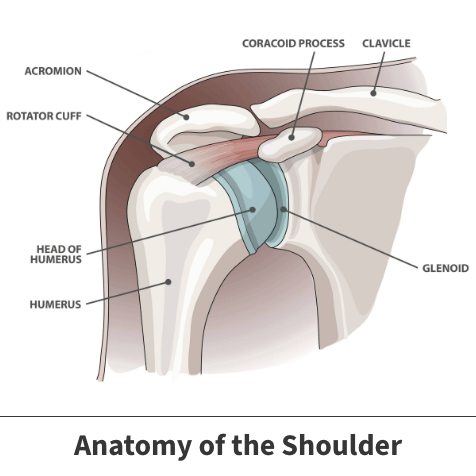
The shoulder is a shallow ball-and-socket joint. It is comprised of the humeral head, a ball-like structure at the top of the upper arm bone, and the glenoid, a shallow socket on the shoulder blade.
The humeral head rests on the glenoid and is held in place by stabilizing tissues including the:
- Labrum: A circular band of cartilage that surrounds the rim of the glenoid, enhancing its depth and stability.
- Capsule: A robust sheet of ligaments and connective tissues that envelops the joint, maintaining its integrity and connecting the ball to the socket.
- Rotator Cuff: A group of four muscles and tendons that connect from the shoulder blade to the humeral head. These provide dynamic stability and facilitate shoulder movement.

Shoulder instability can occur when any of these structures are weakened (atraumatic = not related to a sudden injury) or torn (traumatic = related to a sudden injury).
Multidirectional shoulder instability (MDI) means that the ball moves too far in more than one direction (forwards, backwards, and/or down). This excessive movement can lead to pain and instability.
Unlike unidirectional instability, which involves instability in only one direction (such as forwards or backwards), MDI affects the shoulder joint’s stability in multiple directions, making it more challenging to manage and treat.
Causes of multidirectional shoulder instability
The main causes of MDI include:

- Genetics: Some individuals may have inherently loose joints called “generalized hyperlaxity,” making them more prone to instability. A few of these conditions include Ehler-Danlos syndrome, Marfan syndrome, osteogenesis imperfecta, and hypermobility spectrum disorder.
- Repetitive Overhead Motions: Athletes or individuals engaged in activities like baseball, gymnastics, volleyball, or swimming may gradually weaken the shoulder’s stabilizing structures through repetitive strain and microtrauma.
- Trauma: Although less common, acute injuries such as dislocations or fractures of the shoulder joint can disrupt stabilizing tissues and contribute to instability.
Symptoms
MDI can be difficult to diagnose as it often starts with vague shoulder pain and not a specific injury or traumatic event.
Other common symptoms of MDI include:
- Sensations of Instability: Patients may feel as though their shoulder is slipping out of place, particularly during certain movements.
- Muscle Weakness and Dysfunction: Muscle weakness, numbness, or tingling sensations in the shoulder or arm.
- Recurrent Subluxations or Dislocations: Episodes of partial or complete shoulder dislocation may occur, often in multiple directions.
- Audible Sounds: Some patients may experience catching, popping, or grinding sensations within the joint during movement.

Diagnosis & Treatment
Diagnosing MDI typically involves a comprehensive evaluation, including a thorough medical history, physical examination, and imaging studies such as X-rays, MRI, or CT scans.
Treatment options include non-surgical and surgical options, with non-surgical options being the first ones to try:
- Physical Therapy: The goal of physical therapy is to restore shoulder motion and increase the strength of the rotator cuff and periscapular muscles. Strengthening these muscles helps to stabilize the shoulder and prevent it from re-dislocating or subluxing (partially dislocating)
- Activity Modification: Avoiding or modifying activities that exacerbate shoulder instability, especially overhead or repetitive motions, may be necessary.
- Bracing or Taping: External support, such as shoulder braces or kinesiology tape, can provide additional stability during activities.
- Surgical Intervention: In cases of severe or persistent instability where long-term physical therapy hasn’t helped, surgical options such as arthroscopic stabilization, capsular plication, and ligament reconstruction may be considered.
What are the outcomes?
With appropriate and diligent physical therapy, up to 90% of patients with MDI will experience complete resolution of their symptoms.
For those that do not improve with physical therapy alone, surgery and post-operative rehabilitation offer a successful and reliable treatment option.
Expert Contributor

Dr. Laurel Collings, MD, PGY4 Orthopaedic Surgery Resident, University of Calgary
References
- Jaggi A, Lambert S. Rehabilitation for shoulder instability. British journal of sports medicine. 2010 Apr 1;44(5):333-40.
- Labriola JE, Lee TQ, Debski RE, McMahon PJ. Stability and instability of the glenohumeral joint: the role of shoulder muscles. Journal of shoulder and elbow surgery. 2005 Jan 1;14(1):S32-8.
- Levine WN, Flatow EL. The pathophysiology of shoulder instability. The American journal of sports medicine. 2000 Nov;28(6):910-7.
- Hippensteel, K.J. MD; Uppstrom, Tyler J. MD; Rodeo, Scott A. MD; Warren, Russell F. MD. Comprehensive Review of Multidirectional Instability of the Shoulder. Journal of the American Academy of Orthopaedic Surgeons 31(16):p 871-880, August 15, 2023. | DOI: 10.5435/JAAOS-D-22-00983
- Johnson DJ, Tadi P. Multidirectional Shoulder Instability. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557726/