Tibial Plateau Fractures: the basics
The tibia, or shinbone, is a large bone in the lower leg and one of the most commonly broken bones in the body.
Of all fractures sustained in the body, 1% are tibial plateau fractures.
Anatomy of the knee joint
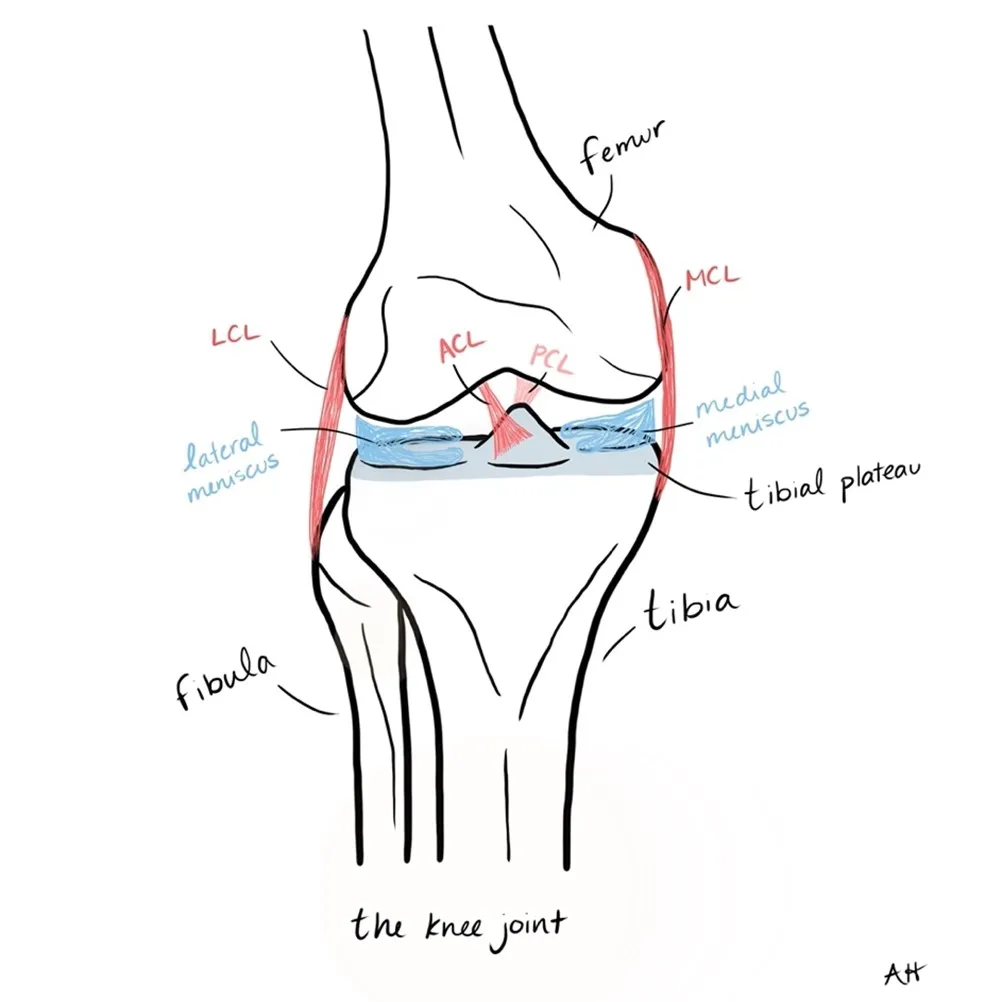
The tibia connects to the femur (or thigh bone) to form the knee joint. The tibia also connects to a bone called the fibula, which is a much smaller bone in the lower leg. The patella, or kneecap, rests over top of the femur and the tibia.
The very top portion of the tibia is known as the tibial plateau. The plateau is a relatively flat part of the bone that acts as the weightbearing platform for the femur and facilitates movement of the femur.
In fact, because the tibial plateau is so large, it bears most of the weight of the body. The fibula, on the other hand, only bears about 15% of body weight.
Several ligaments (connect bone to bone) attach the femur to the tibial plateau. Ligaments, including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and the medial cruciate ligament (MCL), anchor the tibia and femur together. Additionally, several tendons (connect muscle to bone) connect to the tibia. The medial meniscus and lateral meniscus, which are made of a type of cartilage, sit on top of the tibia and act as a cushion for the femur.
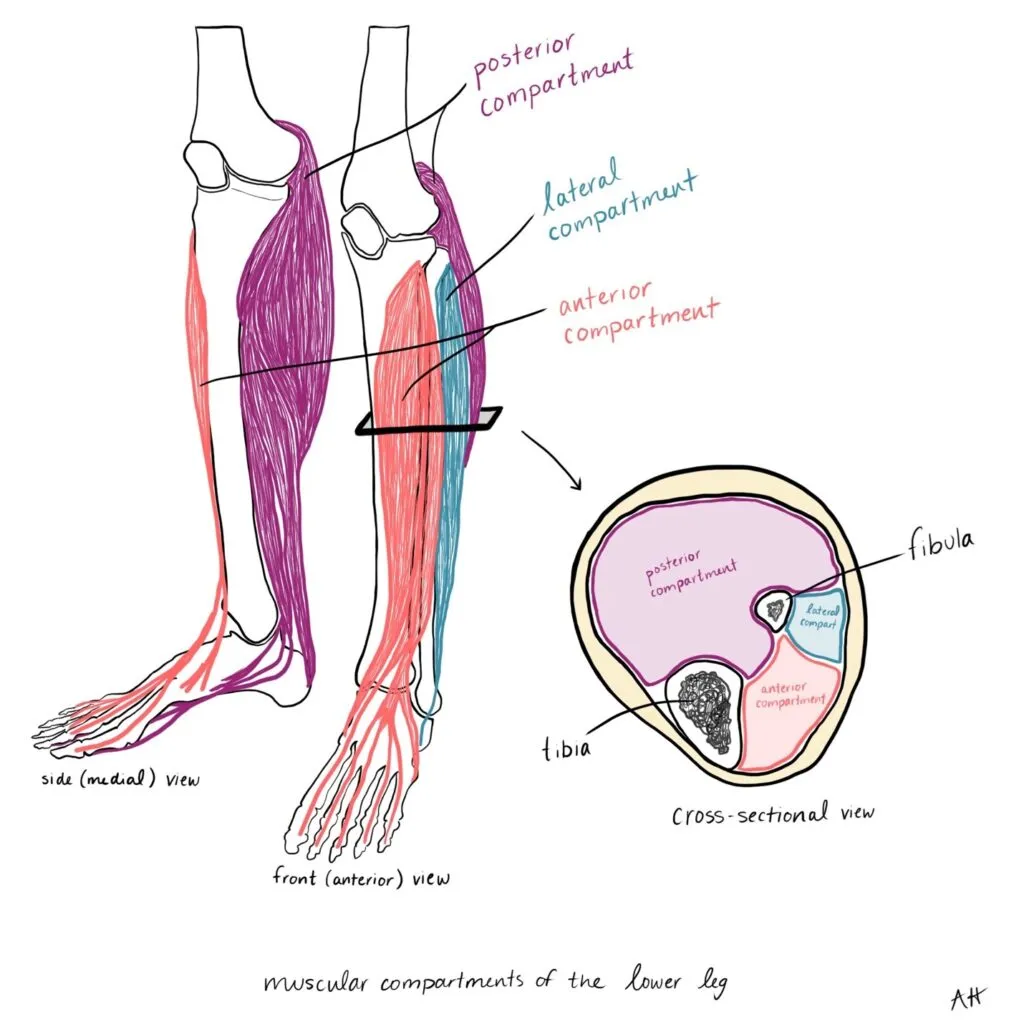
Several nerves and blood vessels that supply the tibia and other parts of the lower leg cross through the knee joint. Additionally, three separate muscular compartments surround the tibia –the anterior, lateral, and posterior compartments. These compartments consist of groups of muscles that are surrounded by a tough sheath known as fascia.
Types of tibial plateau fractures
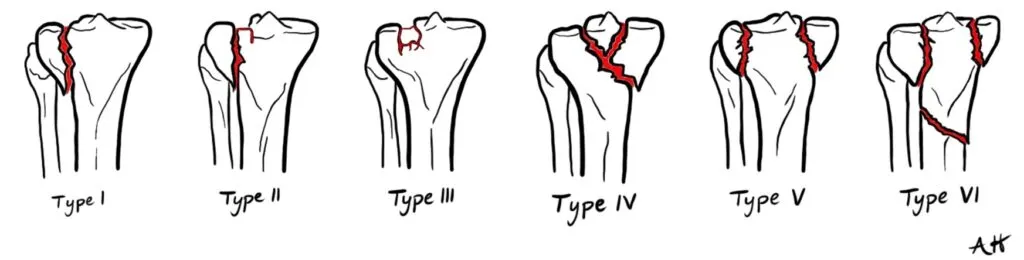
Doctors often differentiate between the type of tibial plateau fracture using a system called the Schatztker Classification.
Schatzker classifications range from I to VI and describe where the fracture occurred and what the fracture looks like. Several other fracture classification systems exist, including the AO/OTA and the Hohl and Moore systems. These systems can be used when the fracture pattern does not fit a Schatzker classification type.
Tibial plateau fractures can occur through either high- or low-energy injury mechanisms.
High-energy mechanisms include a direct blow to the knee from the side, a fall from height, or a motor vehicle collision. They can also occur in sport accidents involving high velocity such as skiing, horse riding, and certain water sports.
High-energy fractures are typically Schatzker Type IV, V, VI, and are generally more complex. Because ligaments, tendons, menisci, nerves, and blood vessels are closely associated with the tibial plateau , injury to these structures is often associated with high-energy tibial fractures. Injury to the ACL, the lateral meniscus, and soft tissue structures in the back of the knee known as the “posterolateral corner” are the most commonly injured, but the PCL, LCL, MCL, and medial meniscus can also be damaged.
Low-energy fractures, on the other hand, occur only in older or weaker bone that is unable to withstand the normal forces applied to the tibial plateau. These types of fractures can occur simply by falling from standing height. Low-energy fractures are most likely to be compression type fractures, classified as Schatzker Type I, II or III. Osteoporosis is a risk factor for these types of low-energy fractures.
A tibial plateau fracture complication – acute compartment syndrome
A very important complication of a tibial plateau fracture is a condition called acute compartment syndrome.
Compartment syndrome is an orthopaedic emergency!
After suffering a tibial plateau fracture, swelling or bleeding may occur within the muscular compartments in the lower leg.
Because the fascia is tough and cannot expand, pressure within the compartments can increase quickly, impeding blood flow to the muscles. If the pressure is not relieved quickly, tissue can die, causing permanent disability or even loss of the leg.
Symptoms of compartment syndrome include severe pain, especially when the muscles are stretched or moved. You may also feel a tingling or burning sensation, and the muscles may feel tight or full. Surgery is the only way to relieve the pressure within the compartments. The surgeon will cut open the fascia in the affected compartment – a procedure called a fasciotomy. If the pressure is not relieved immediately when the fascia is cut, the surgeon may leave the incision open until the inflammation in the muscle comes down. While leaving the wound open is necessary to allow the inflammation to settle and to avoid permanent damage, this procedure significantly increases the risk of infection.
How is a tibial plateau fracture diagnosed?
When diagnosing a tibial plateau fracture, the doctor will ask about the mechanism of injury, or how you injured yourself. The doctor will also ask about any other risk factors you may have – if you have osteoporosis, and if you smoke or drink alcohol.
A doctor will then examine the injury, looking at the skin for any wounds or lacerations, or any obvious deformities or swelling around the knee. They will feel the injury to determine where the pain is and test the range of motion of the knee. The doctor may also look for fluid in the knee joint and may take a small needle to pull some fluid out of the joint, a technique called “aspiration.” The fluid may give clues as to what parts of the bone are damaged. Normally, blood and fat are contained within the tibia, (think of bone marrow in a beef bone). If the tibia is broken, blood and fat may leak out and into the joint space, which can be seen on aspiration.
It is also important for the doctor to assess neurovascular function – the nerves and blood vessels that run close to the knee and supply the lower leg. The doctor will assess sensation and motor function in the lower legs and feet to test for nerve damage. They will also feel for a pulse on the surface of the foot and the ankle to assess blood vessel damage.
The doctor will also test the integrity of the ligaments and menisci of the knee to determine if these structures have been damaged. This is sometimes difficult to do if there is significant swelling and pain, so the doctor may give a local anesthetic to properly assess the knee.

Finally, the doctor will screen for acute compartment syndrome, making sure there isn’t excessive pain when the lower leg muscles are stretched. They will also test blood flow by checking the pulses in the ankle and foot.
If a tibial plateau fracture is suspected, the doctor will order X-rays to help determine the Schatzker classification of the fracture. The doctor may also order a CT scan, which will give a clearer picture of the bone fracture. This helps the doctor decide if surgery is necessary, and if so, what surgical approach to take. If the doctor suspects that the ligaments and menisci are damaged, they will also order an MRI, which will give the doctor a clearer picture of soft tissue (ACL, PCL, meniscus) damage.
Treatment of tibial plateau fractures
The main goals of treating a tibial plateau fracture are to restore alignment of the limb, restore knee stability, and ensure painless functional range of motion at the knee joint.
In the long run, the goal of treatment is to decrease the risk of developing osteoarthritis. The risk of post-traumatic osteoarthritis is highest when knee stability is not restored properly or there is malalignment of the joint. Because tibial plateau fractures vary widely in severity and complexity, there is no “one-size -fits-all” treatment strategy. Surgery may or may not be required.
Non-surgical treatment
In general, surgery is not required when the fracture is “minimally displaced,” meaning the bone is broken but has not moved out of alignment, and there is no injury to the ligaments and menisci. Also, surgery may not be recommended in elderly or sedentary people.
Typically, if surgery is not required, a cast brace can be applied within 7 to 10 days after your injury. Until the cast is applied, weight-bearing on the injured leg must be avoided. If you are treated non-surgically, the doctor will follow-up with you approximately every 2 weeks for X-rays to make sure the bone is healing properly. At 12 weeks, the cast brace can be removed if “bony union” has occurred, meaning that the fracture has healed. Rehabilitation should focus on quadriceps and hamstring strength. Activities like running should not be allowed until 4 to 6 months post-injury.
Surgical treatment
Most tibial plateau fractures will require surgery to preserve knee function. Several techniques can be used based on the type of fracture, or Schatzker classification, and the degree of ligament and meniscal damage.
The goal of surgical treatment is to realign the fractured bones and fix them in place until the bone heals. If there is ligament and meniscus damage, these will also need to be repaired surgically.
Surgery can be done arthroscopically or using techniques known as “open reduction and internal fixation,” or “external fixation.”
Arthroscopy is minimally invasive technique that involves placing a camera into the knee joint through a small incision and is commonly used for less complex fractures, including Schatzker types I, II, III, and sometimes IV. Through small incisions, the surgeon will use pins inserted into the bone to realign the fractured bone parts. If there is a depression fracture, like in Schatzker type II and III, the surgeon can “push” the depressed portion of the bone back in place. Ligament and meniscus repair can also be done arthroscopically.
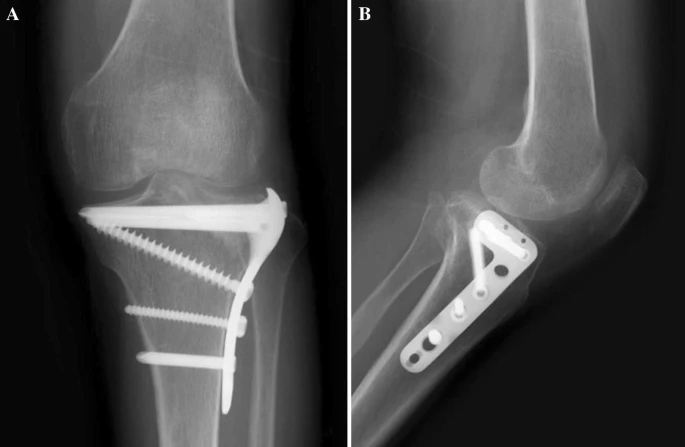
Open reduction and internal fixation is a more invasive procedure and is generally used in Schatzker types IV, V, and VI. Usually, a plate and several screws are used to stabilize the fracture.
External fixation may be recommended in complex fractures where there is significant bone and soft tissue damage (mainly Schatzker type V and VI fractures). This technique involves passing rods and wires through the fracture inside the body and then attaching them to a stabilizing device that is located outside of the body.

In some fractures, there is significant damage to the bone where it becomes compacted and leaves a space that needs to be filled. When this is happens, something called a bone graft can be used. A bone graft involves either taking bone from yourself (usually the hip bone), from a cadaver, or using a synthetic graft.
Risks and complications with surgical treatment of tibial plateau fractures
While there are several risks and complications that can arise with tibial plateau surgery due to its complexity, the benefits of surgery greatly outweigh the risks of complications.
Unfortunately, post-traumatic osteoarthritis is a relatively common occurrence after tibial plateau surgery (25-35% of cases). The development of osteoarthritis varies with the type of fracture and the type of surgery performed. A misaligned joint or instability in the joint increase the risk for osteoarthritis. It is also more common if the meniscus was damaged during the injury. A total knee replacement may be recommended in older patients, while in young patients, surgery to fix joint alignment is usually the best option.
After surgery, knee stiffness and decreased range of motion are common complications of surgery and occur in 10-25% of cases. Knee stiffness is amplified if the leg is immobilized after surgery. For this reason, it is very important to work with a physiotherapist to mobilize the knee safely. If knee stiffness persists for more than 12 months following surgery, a second surgery can be performed to help improve mobility in the joint.
As mentioned earlier, acute compartment syndrome can occur following a tibial plateau fracture. This occurs in 7-20% of cases but is more likely with high-energy fractures. The likelihood of compartment syndrome increases as the energy and complexity of the fracture increases. The surgeon will immediately perform a fasciotomy to release the muscular compartment.
As with any surgery, infection is also a risk and can occur in approximately 2-11% of cases; particularly at the incision site but also deep within the tissue. To mitigate this risk, you will be given antibiotics after surgery. Signs of infection include inflammation, fever, general malaise, flushing, or pus at the incision site. Infections can occur anytime, sometimes more than 10 weeks after surgery. This is a serious complication and will often require more surgical procedures and a course of antibiotics. If the fracture has healed, hardware (screws and plates) may have to be removed to resolve the infection. If the fracture has not healed, the hardware will be left in, but any loose screws or stitches will be removed.
Malunion is a rare complication and occurs in 2-4% of cases. It occurs when the bone doesn’t heal properly. With malunion, osteoarthritis in the knee can occur, or the lower limb can become misaligned, resulting in discomfort or mobility problems. In young, active patients, malunion is often fixed with another surgery. In older patients, a total knee replacement might be necessary. Another rare complication is known as non-union and occurs in less than 1% of surgeries. This is when the bones do not show signs of healing after 9 months.
Rehabilitation and recovery from a tibial plateau fracture
After tibial plateau surgery, rehabilitation and physiotherapy are extremely important.

A tibial plateau fracture can be a serious injury and the road to recovery can be long. Adhering to rehab guidelines will ensure the best outcomes. As with most rehab protocols, there is no one-size-fits-all formula, and every rehab plan should be individualized based on the type of surgery that was performed, pain level, age, overall fitness, and patient goals.
Range of motion exercises should be performed as soon as possible following surgery. As long as pain is well controlled, these exercises can be performed as early as 1- or 2-days post-surgery.
The use of a knee brace is recommended (except where an external fixator surgery took place, and a knee brace cannot be worn). It is not recommended that a knee brace is used for more than 2 weeks, but this depends on the degree of soft tissue damage. Most surgeons will recommend that, following an internal fixation surgery, partial weight-bearing should occur for about 4 to 6 weeks following surgery. However, this recommendation can vary based on pain levels. Some studies have shown that the early partial weight-bearing results in earlier full weight-bearing. X-rays can confirm that the bone has healed, and it is safe to fully weight-bear. With an external fixation surgery, it is usually recommended that weight-bearing occur early.
Return to activity and sport
The timing for returning to sport following a tibial plateau fracture depends on many factors – if surgery was performed, what type of surgery was performed, if ligaments and menisci were injured, and if the patient followed physiotherapy and rehabilitation protocols.
As you can imagine, more severe fractures generally require a longer period of healing before return to sport is safe.
On average, most people can return to sport after about 7 months, but this timeline can range from anywhere between 6 and 12 months. These guidelines, however, should be taken with a grain of salt and should be highly individualized.
Contributing Expert

Annika Hicks, second year medical student (class of 2025) at UBC Southern Medical Program (Kelowna)
References
Gupton M, Munjal A, Kang M. Anatomy, Bony Pelvis and Lower Limb, Fibula. 2022 May 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29261984.
Elsoe R, Larsen P, Nielsen NP, Swenne J, Rasmussen S, Ostgaard SE. Population-Based Epidemiology of Tibial Plateau Fractures. Orthopedics. 2015 Sep;38(9):e780-6. doi: 10.3928/01477447-20150902-55. PMID: 26375535.
Ramponi, Denise, McSwigan, Tara. Tibial Plateau Fractures. Adv. Emerg. Nurs. J.. 2018;40(3):155-161. doi:10.1097/TME.0000000000000194.
Adams JDJ Jr, Loeffler MF. Soft Tissue Injury Considerations in the Treatment of Tibial Plateau Fractures. Orthop Clin North Am. 2020 Oct;51(4):471-479. doi: 10.1016/j.ocl.2020.06.003. Epub 2020 Aug 12. PMID: 32950216.
Kfuri M, Schatzker J. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 2018 Dec;49(12):2252-2263. doi: 10.1016/j.injury.2018.11.010. PMID: 30526924.
Schneiderman BA, O’Toole RV. Compartment Syndrome in High-Energy Tibial Plateau Fractures. Orthop Clin North Am. 2022 Jan;53(1):43-50. doi: 10.1016/j.ocl.2021.09.001. Epub 2021 Oct 28. PMID: 34799021.
McClellan RT, Comstock CP. . Evaluation and treatment of tibial plateau fractures. Current Opinion in Orthopedics. 1999; 10 (1): 10-21.
Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Rev. 2017 Mar 13;1(5):225-232. doi: 10.1302/2058-5241.1.000031. PMID: 28461952; PMCID: PMC5367528.
Burdin G. Arthroscopic management of tibial plateau fractures: surgical technique. Orthop Traumatol Surg Res. 2013 Feb;99(1 Suppl):S208-18. doi: 10.1016/j.otsr.2012.11.011. Epub 2013 Jan 21. PMID: 23347755.
Gálvez-Sirvent E, Ibarzábal-Gil A, Rodríguez-Merchán EC. Complications of the surgical treatment of fractures of the tibial plateau: prevalence, causes, and management. EFORT Open Rev. 2022 Aug 4;7(8):554-568. doi: 10.1530/EOR-22-0004. PMID: 35924649; PMCID: PMC9458943.
Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006 Jun;37(6):475-84. doi: 10.1016/j.injury.2005.06.035. Epub 2005 Aug 22. PMID: 16118010.
Tibial Plateau Fractures – Trauma – Orthobullets. (2023). Retrieved 15 January 2023, from https://www.orthobullets.com/trauma/1044/tibial-plateau-fractures
Iliopoulos E, Galanis N. Physiotherapy after tibial plateau fracture fixation: A systematic review of the literature. SAGE Open Med. 2020 Oct 14;8:2050312120965316. doi: 10.1177/2050312120965316. PMID: 33133602; PMCID: PMC7576901.
Robertson GAJ, Wong SJ, Wood AM. Return to sport following tibial plateau fractures: A systematic review. World J Orthop. 2017 Jul 18;8(7):574-587. doi: 10.5312/wjo.v8.i7.574. PMID: 28808629; PMCID: PMC5534407.
Campbell’s Operative Orthopaedics, Fourteenth Ed. Azar, Frederick M., 2021, Elsevier Inc.