Hamstring Tendon Autograft
Autografts in ACL reconstruction are tendons harvested from the patient’s own body at the beginning of the procedure and prepared as a tissue graft that can be inserted into the knee during the same procedure in an attempt to restore the normal anatomy of the ACL.
Autograft tendons are the most commonly used of the different types of grafts available.
—– Learn more about the other graft types here —–
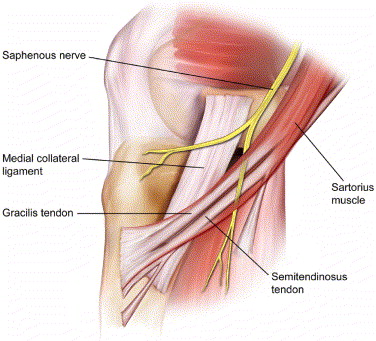
Of these, the most common autograft tendons are the hamstring tendons, specifically the semitendinosus (ST) and gracilis tendons (GT), which are part of the medial hamstring group.
If the ST, which is the larger of the two tendons, is long and wide enough, it can be used alone. If not, the GT can be added to the graft.
Studies show that hamstring grafts with a diameter (width or thickness) of at least 8 mm have a significantly lower risk of re-tear after returning to sports and activities.
If using the ST alone, it must at least be tripled or quadrupled to achieve an adequate graft. However, the more it is folded over, the shorter the graft becomes, and a graft must be at least 7 cm long to be useful.
In most cases, using a doubled ST and a doubled GT together results in an adequate graft.
In some cases, both tendons together do not provide for a large enough graft, and additional tissue must be added to it – usually an allograft tendon. This is called a hybrid graft, and the decision to add this to the graft is made intra-operatively (during surgery).
In some centres, a synthetic augment (InternalBrace) is used to reinforce the graft in this scenario, but this is not yet standard practice amongst our group of surgeons at Banff Sport Medicine.
Studies show that small hamstring tendon size is correlated with short stature, low BMI and female gender. If you are a petite female, your ST and GT may not be large enough for an adequate sized graft and your surgeon may recommend another graft option.
Advantages of the hamstring autograft
There are several advantages of using a hamstring graft and that is reflected in the statistics, which show it is the most widely used graft in the world.
Human cadaver studies confirm that a 4 stranded hamstring graft is the strongest autograft available.
A native or normal ACL has a load to failure (strength) which ranges from 1,725 – 2,160 N (newtons), whereas a 4 stranded hamstring graft has a strength of up to 4,300 N.
Unfortunately, this is the time zero strength, or the strength of the graft when it is first implanted.

Animal studies show that the graft never achieves more than 50-60% of the native ACL strength at the end of the healing process. There is no way to confirm if this is actually the case, as this type of study is not possible in humans.
Another significant advantage of the graft is that because it does not involve the extensor mechanism (quadriceps muscle), there is earlier and more complete return of knee extensor strength after surgery.
Studies involving functional testing after ACL reconstruction show that patients with stronger quadriceps muscle strength perform significantly better, and studies specifically comparing functional performance between hamstring tendon autograft and patellar tendon autograft show that the hamstring group often performs better.
Also, the incisions used during an ACL reconstruction with hamstring autograft are small and less disfiguring.
Disadvantages of the hamstring autograft
The disadvantages of using a hamstring autograft are also important for the patient to be aware of.
Studies have shown that although the risk of post-operative wound infection after ACL reconstruction is low (< 1%), the use of hamstring autografts is associated with a higher risk of post-operative wound infection as compared to the other autograft options.
Soaking the graft in an antibiotic solution during surgery prior to implantation can significantly decrease this risk.
Another disadvantage is that some patients are left with some residual hamstring muscle weakness long term. This involves mainly knee flexion weakness at higher flexion angles (90 degrees or more) and is more pronounced when both the ST and GT are used, as compared with using the ST alone.
Several studies have shown that both tendons can fully regenerate, but this occurs in only 75-85% of cases.

This residual weakness may be a problem in some sports such as gymnastics, wrestling and martial arts, although there are no clinical studies that confirm this.
Another consequence of incomplete regeneration of the ST and GT relates to medial knee instability.
Besides knee flexion strength, these tendons also act as dynamic stabilizers of the medial side of the knee.
Because of this, your surgeon may not recommend this graft for you if you have any degree of medial collateral ligament (MCL) laxity (looseness). However, in this situation, another option is to harvest the hamstring tendons from the opposite leg.
Two relatively common disadvantages of using hamstring autograft are related to the tendon harvest site: hamstring muscle strains and sensory nerve abnormalities.
About 25% of patients will experience a sudden, painful pop or pulling sensation at the back of their thighs within the first 6 weeks post-operatively. This is usually precipitated by a sudden knee flexion contraction as when pulling your shoe off using the opposite foot. This represents a minor hamstring muscle strain which resolves spontaneously within a week or so in most cases, and does not adversely affect the outcome of the surgery.
Also, up to 50% of patients will experience some degree of numbness in their operative leg adjacent to the tendon harvest incision. In some cases, the numbness can extend down the leg and into the medial side of the ankle, or can even cross over onto the lateral side of the lower leg. In the majority of patients this numbness will slowly resolve over time. It may completely resolve, and if not, is not bothersome to most people.
Contributing expert

Dr Greg Buchko, Orthopaedic Surgeon






