Patellar Tendon Autograft
The patellar tendon autograft is the second most common choice used for an ACL reconstruction autograft after the hamstring tendon autograft.
This graft is also known as a bone-patellar tendon-bone (BPTB) graft.
—– Learn more about the other types of grafts here —–
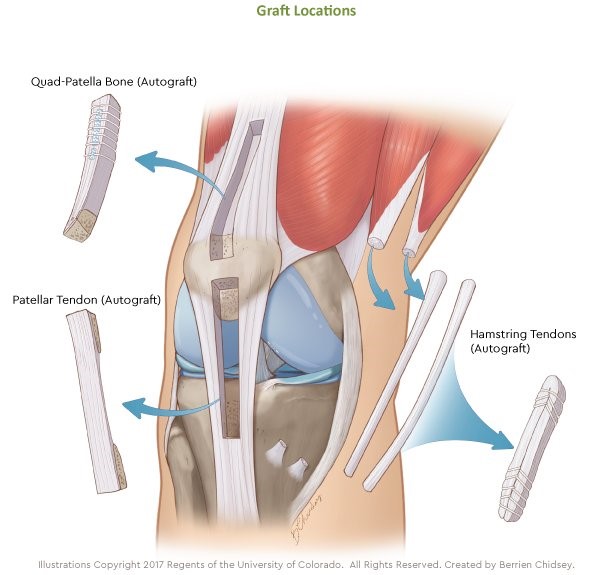
It is harvested from the central one-third of the patellar tendon along with a bone block from the patella at one end and a bone block from the tibia (shin bone) at the other end (the tendinous portion of the graft is too short to use alone).
It is usually 9-10 mm in width and 8-9 cm in length. However, as is the case with the hamstring graft, smaller female patients often do not have a wide enough patellar tendon to make this graft option feasible. If this is the case, your surgeon may recommend another graft option.
Human cadaver studies have shown that harvesting a 10 mm wide graft from a 30 mm wide patellar tendon (average width) will weaken it by 25%, so if the tendon is even narrower than 30 mm, you are increasing the risk of patellar tendon rupture as a complication of the surgery.
Fortunately, clinical studies show that the central defect created in the patellar tendon after harvest will completely regenerate by one-year after surgery, so that the patellar tendon strength most likely fully recovers by that point.
Advantages of the patellar tendon autograft
For many years, this graft has been considered by some to be the “gold standard” when it comes to ACL grafts for the following reasons (truthfully, there is really no one autograft that is significantly superior to the others). Because there is a block of bone at each end, the graft will heal more quickly to the femoral and tibial bone tunnels drilled to accept the graft.
Animal studies show that the patellar tendon graft will heal in the bone tunnel at an average of 6 weeks, whereas a soft tissue graft, like the hamstring graft, will take an average of 12 weeks.
—– Learn more about the hamstring tendon autograft here —–
Some surgeons feel that this may aid in speeding up recovery, but this is probably not the case based on more recent comparison studies which looked at thousands of patients.
The patellar tendon is also a strong graft, with human cadaver studies showing a load to failure of up to 3,000 N, although there is no reason to assume that it is any stronger than an adequately sized hamstring graft at the end of the healing process.

More recent large systematic reviews involving thousands of patients comparing patellar tendon to hamstring tendon grafts do show a slightly lower re-tear rate when using patellar tendon grafts with the difference being about 1-2 %.
Some of these studies also show a slight difference with regard to patellar tendon grafts having less laxity, but no difference with regard to return to sports rates or patient reported outcomes (subjective outcomes).
There is some evidence to show that a patellar tendon graft may be the optimal graft in young females and patients with generalized ligamentous laxity (loose ligaments).
Disadvantages of the patellar tendon autograft
The disadvantages of the patellar tendon autograft are mainly related to complications at the harvest site. Numerous studies show that there is a significantly higher risk of anterior knee pain and kneeling pain with this graft compared to others.

Patients whose occupation involves a lot of kneeling and squatting should consider a different graft option.
As with hamstring grafts, harvesting patellar tendon grafts can result in skin numbness. This occurs to some degree in most cases, but usually in just a small to moderate sized area lateral to the incision, which is significantly longer than a hamstring graft incision.
Also, because bone from the patella is taken with the graft, there is a chance this could weaken the bone resulting in a fracture. However, the risk of this is low (<1%).
There is also a tiny risk (0.25%) of experiencing a rupture of the patellar tendon after graft harvest. Many studies have also found that the risk of developing osteoarthritis after ACL reconstruction with patellar tendon is significantly higher than when other grafts are used.
Also, many studies have shown that the recovery of knee extensor, or quadriceps muscle strength, is more prolonged and often incomplete after ACL reconstruction with patellar tendon when compared to ACL reconstruction with hamstring tendon autograft.
Finally, several studies have shown that it is more difficult to regain full knee extension post-operative with use of this graft, and this may also contribute to the delay in quadriceps muscle recovery.
Contributing expert

Dr Greg Buchko, Orthopaedic Surgeon







