Distal Radius Fractures: The Basics
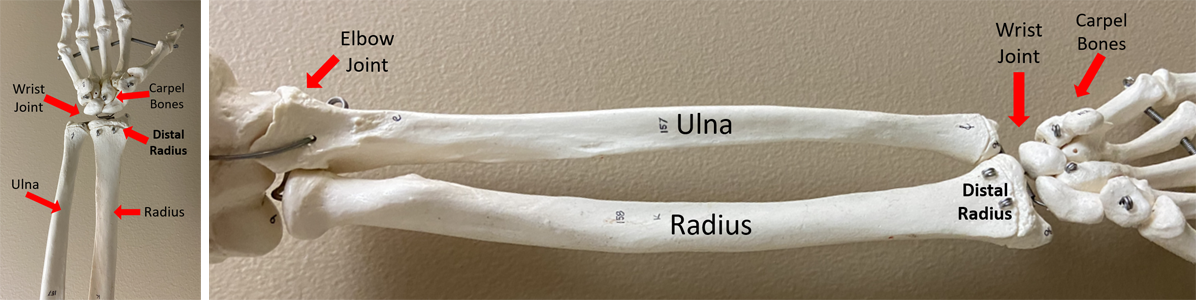
A distal radius fracture is a break in one of the two forearm bones, the radius, near the wrist joint. Hence, this type of fracture can also be referred to as a wrist fracture or broken wrist.
This type of fracture is a common injury often occurring due to either a fall on an outstretched or flexed hand, or from a direct blow to the wrist, such as from a car, bike, or ski/snowboard accident. This type of wrist fracture is also a common type of fracture in children under 16 and in older women with osteoporosis.
Types of distal radius fractures
Distal radius fractures can vary in severity from minor fractures that require a cast, to more complex fractures that require surgery.
Depending on how the distal radius breaks, the fracture can be called a Colles or Smith fracture.
Colles Fracture
Colles fractures are the most common type of distal radius fracture. In a Colles fracture, the distal end of the radius bone typically breaks due to a fall on an outstretched hand. The fracture results in the broken bone fragment pushed towards the back of the wrist resulting in a characteristic “dinner fork” deformity (this type of fracture results in a distinct “bump” in the wrist that is similar to the neck of a fork).
Smith Fracture
A Smith fracture may also be called a Reverse Colles fracture, and is less common than the Colles. Smith fractures typically occur due to a fall onto a flexed wrist. In this type of fracture, the broken bone fragment is pushed towards the palm side of the wrist.
How are distal radius fractures treated?
Treatment typically begins in the emergency department after X-rays are done to assess the extent of damage to the bones. The radius bone is then re-aligned and cast.
Depending on the severity of the fracture and how well aligned the bone is after casting will influence how the fracture is then managed and treated.
Non-Surgical Treatment
For less severe fractures where the bones are not significantly moved out of place, a cast is used to immobilize the wrist after realignment. This allows the bones to heal naturally over time.
This treatment option will involve regular x-rays to ensure proper healing and alignment of the wrist.
Surgical Treatment
In cases where the bone is severely displaced (and can’t be treated with a cast) or the fracture is unstable or not adequately aligned even after being in a cast, surgery may be recommended.
Surgery involves realigning the bones of the wrist and using plates and screws to hold them in place. The surgeon will discuss the specific surgical procedure and the expected outcomes. Generally, the operation lasts 60 minutes with an incision on the inside of the wrist.
What is the recovery process?
How long recovery takes will depend on the type and severity of the distal radius fracture and the chosen treatment method.
You may need to wear a cast or splint to support the healing process. Pain and swelling are common initially but should gradually improve with time. It is advisable to practice standard comfort and pain reduction strategies with rest, ice, elevation, and analgesia in the initial period tapering as pain improves. Continue to move your elbow and fingers to help reduce stiffness and aid recovery.
Generally, non-operative management involves cast immobilization for 6 weeks then transitioning into a splint for an additional 2 weeks. This transition period allows for range of motion of the wrist joint while also providing additional protection. You can expect significant stiffness in the wrist after removal of the cast. This improves with use and range of motion exercises.

A broken bone takes roughly 6 weeks to heal but it is still at a higher risk of re-injury until the surrounding muscles have had time to strengthen. Thus, it can take up to 3 months before you can return to full activities and 1 year until full recovery. Most individuals begin a slow return to function, working on strength and range of motion, at 6 weeks from injury. This is also the time when you can begin increasing your weightbearing, using pain as your guide.
Distal radius fractures that require surgery also follow a similar timeframe for recovery with avoidance of weightbearing and high impact activity for 6 weeks followed by strengthening and a slow return to activity after this time. After your operation you may be placed in a splint for 2 weeks to allow rest of the soft tissues and healing of your surgical site. After the initial two weeks you can often begin range of motion exercises maintaining non weight bearing status.
Potential challenges after a distal radius fracture
- Decreased range of motion: It is common to have stiffness in the wrist after surgery or wearing a cast. It is important to follow recommendations for range of motion to gain back function and motion of the wrist. Flexion and extension are the slowest to return with improvements in motion expected up to 6 – 12 months. The largest improvements of range of motion will be seen in the first 6-12 weeks after surgery. On average, individuals will regain 90% of their range of motion when compared to their uninjured side.
- Hardware Irritation: If surgery was required, there can be irritation of the surrounding structures which requires removal of the plate and screws. Roughly 10% of individuals require plate removal most commonly due to irritation of one of the wrist and hand tendons (the extensor tendon).
- Infection: The risk of infection is low with a <1% infection rate.
- Post traumatic arthritis: There is an increased risk of arthritis in fractures that extend into the joint. This rate is reported to be anywhere from 30-97% of individuals. Being of older age at the time of injury is associated with an earlier onset of arthritis.
What does rehabilitation involve?
Rehabilitation plays a crucial role in recovering from a distal radius fracture.
Your work begins after removal of the cast with a goal to achieve full range of motion.
Range of motion and strengthening exercises will help to achieve this goal with the aim to:
- Regain strength and range of motion in your wrist and hand with range of motion exercises focusing on flexion, extension, pronation, and supination (moving the wrist through it’s range of motion).
- Reduce pain and stiffness.
- Improve your ability to perform everyday activities.
A physiotherapist may be recommended to give guidance through this process.
Expert Contributor

Jarrett Moore MD MSc, PGY4 Orthopaedic Surgery Resident, University of Calgary
References
1. Mauck BM, Swigler CW. Evidence-Based Review of Distal Radius Fractures. Orthop Clin North Am [Internet]. 2018;49(2):211–22. Available from: https://doi.org/10.1016/j.ocl.2017.12.001
2. Porrino JA, Maloney E, Scherer K, Mulcahy H, Ha AS, Allan C. Fracture of the distal radius: Epidemiology and premanagement radiographic characterization. Am J Roentgenol. 2014;203(3):551–9.
3. Dillingham C, Horodyski M, Struk AM, Wright T. Rate of Improvement following Volar Plate Open Reduction and Internal Fixation of Distal Radius Fractures. Adv Orthop. 2011;2011:1–4.
4. Seigerman D, Lutsky K, Fletcher D, Katt B, Kwok M, Mazur D, et al. Complications in the Management of Distal Radius Fractures: How Do We Avoid them? Curr Rev Musculoskelet Med. 2019;12(2):204–12.






