The Role of Functional Testing Following Knee Ligament Surgery
Did you know the knee joint is the largest joint in the body?
It’s important for almost every movement, from standing, keeping your balance, walking, running, jumping, swimming and more!
The knee is made up of many important components such as cartilage, like the meniscus and articular cartilage, and ligaments including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). These ligaments work together to stabilize the knee joint.
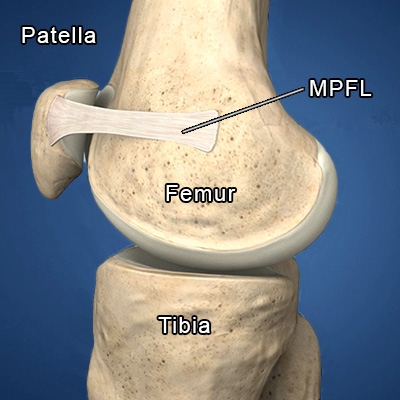
Another important knee ligament is the medial patellofemoral ligament (MPFL). This ligament connects the inner edge of the kneecap (patella) to the thigh bone (femur). Its main function is to stabilize the kneecap.
Injury to these ligaments is common, particularly to the ACL, which is the most injured knee ligament.
While some knee ligament injuries can heal on their own, surgery is often used to repair or reconstruct torn ligaments.
Some of the most common knee ligament surgeries carried out by the orthopaedic surgeons at Banff Sport Medicine include reconstructions of the ACL, PCL and MPFL.
After reconstructive surgery, patients should follow a comprehensive rehabilitation program to restore their knee function and enable a safe return to sport and physical activity with a reduced risk for additional injury.
During rehabilitation, patients are tested and assessed at regular time points to assess how their rehabilitation is going and if they are ready to return to sport and activity.
Whether or not patients are ready will depend on several factors. These include healing of the reconstructed graft, time from surgery, mental readiness, and the ability to pass a battery of functional assessments, such as the ones conducted at Banff Sport Medicine’s Functional Testing Clinics where patients can be tested at 6-, 12- and 24-months after surgery.
The importance of Functional Testing
Functional testing provides crucial information, such as:
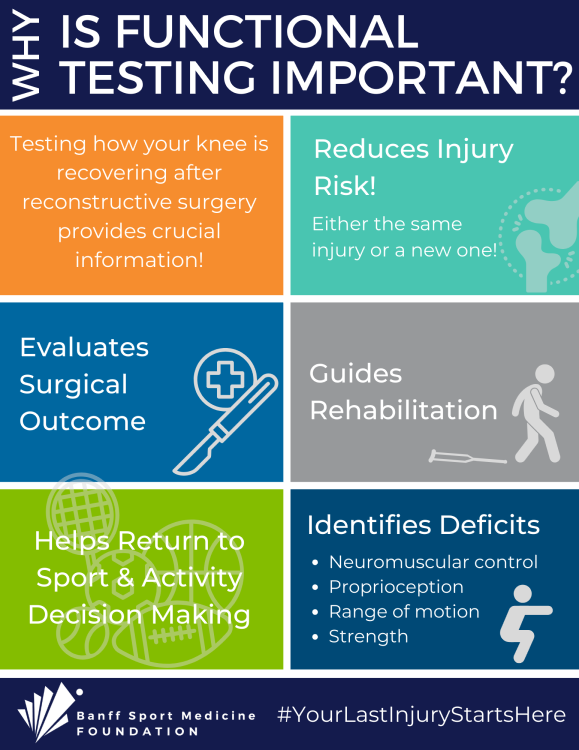
Evaluation of Surgical Outcome: Functional tests allow the surgeon to assess the success of surgery in restoring stability and function to the knee joint. Measurements, such as range of motion, muscle strength, and joint stability, provide valuable feedback on the effectiveness of the reconstruction.
Identifying Deficits & Guiding Rehabilitation: Regular assessment using functional tests helps to identify specific deficits in neuromuscular control (how muscles activate), proprioception (body sense), strength, and movement patterns that may contribute to impaired knee function and increased risk of re-injury. By pinpointing these gaps, rehabilitation programs can be tailored to address individual needs. For example, clinicians can prescribe targeted exercises and interventions aimed at restoring normal movement patterns, improving strength and proprioception, and enhancing overall function. This feedback can also help motivate patients and ensures that rehabilitation goals are being met.
Return to Sport & Activity Decision-Making: Another critical aspect of rehabilitation is determining when an individual is ready to return to sports or high-level activities safely. Functional testing plays a crucial role in this decision-making process by assessing the readiness of the knee joint to withstand the demands of sport-specific movements. Tests such as the hop tests, agility drills, and cutting maneuvers provide valuable information on how well a patient’s recovery is going. This helps the clinician make an informed decision regarding the timing (when) and progression (how) the patient should return to sport and activity, reducing the risk of re-injury.
Injury Risk Reduction: Beyond restoring function and enabling a return to sport and activity, functional testing can also help reduce the risk of future knee injuries. By addressing underlying biomechanical deficits and movement dysfunctions, rehabilitation programs can enhance neuromuscular control, improve landing mechanics, and promote joint stability, thereby mitigating the risk of re-injury or other future injuries.
What to expect during Functional Testing
WATCH this short video on BSM’s Functional Testing Clinic
Range of Motion: Assessing the range of motion of the knee joint is crucial to monitor postoperative progress and identify any limitations that may require intervention. Achieving full range of motion is essential for restoring normal knee function and preventing complications such as stiffness.
Strength Testing: Evaluating the strength of the quadriceps, hamstrings, and other muscles surrounding the knee is essential for assessing muscle imbalances and identifying areas of weakness that may predispose the patient to reinjury or recurrent instability (particularly for those patients that have undergone MPFL reconstruction to treat patella instability).
Dynamic Stability: Dynamic stability tests, such as the single-leg squat or hop tests, assess the ability of the knee joint to withstand functional activities and movements. These tests provide valuable information about the effectiveness of the reconstructed ligament in stabilizing the knee during dynamic movements. These tests also simulate the demands placed on the knee during sports-related activities and provide valuable insights into functional performance and readiness to return to activity.
Proprioception: Proprioception refers to the body’s ability to sense the position, movement, and orientation of its limbs in space. Impaired proprioception can affect balance and coordination, increasing the risk of falls and injury. Assessing proprioceptive abilities can help identify deficits that may require targeted rehabilitation interventions.
Overall, functional testing and assessments at regular intervals are essential components of rehabilitation after surgery. By assessing how the knee (and overall body) is functioning, as well as a person’s strength and stability, clinicians can design individualized treatment plans, monitor progress, and determine a patient’s readiness to return to sports and daily activities.
Functional testing also enhances patient outcomes, reduces the risk of additional injury, and promotes long-term joint health and performance. As such, prioritizing functional testing throughout the rehabilitation process is essential for optimizing recovery and facilitating a safe return to an active lifestyle.







