PRP in Sport Medicine: The Basics
What is platelet-rich plasma therapy?
Platelet-rich-plasma (PRP) therapy is a treatment used for musculoskeletal (bone and joint) injuries that has been gaining popularity in recent years. It involves using the patient’s own blood to promote healing in a specific area of the body, although the exact way that PRP works isn’t fully understood.
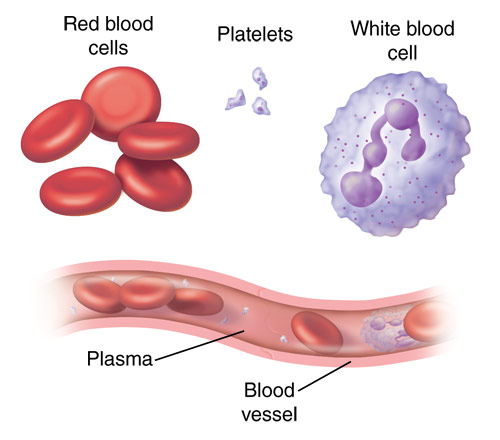
PRP consists of two main parts – plasma (the liquid part of the blood) and platelets.
Platelets, also called thrombocytes, are cells made in the bone marrow that help form blood clots and prevent excessive bleeding. Platelets contain many growth factors and small proteins called cytokines that are very important in the healing of injuries.
In PRP preparations, the platelets are at a much higher concentration than is typically found in the blood (5 to 10 times greater).
Some formulations also include increased concentrations of white blood cells (WBCs). These preparations utilize the inflammatory nature of WBCs to create a larger inflammatory response in the area it is injected which can further promote healing in some conditions and injuries.
The basic idea behind PRP is to increase the amount of growth factors and other proteins and cells to a specific area of the body to accelerate the healing process.
How does PRP therapy work?
PRP preparations are obtained from a patient’s own blood and can vary greatly as there is still no accepted standard on the ideal preparation method.
In general, the process involves:
Preparing for PRP therapy
In preparation for PRP injections, patients are asked to stop certain medications and supplements 2-weeks prior. These include non-steroidal anti-inflammatories that can thin the blood (Ibuprofen, Aleve, Naproxen, Aspirin, Motrin, Voltaren, and Diclofenac) and supplements such as fish oil and flaxseed oil.
For a full list of supplements, read the Banff Sport Medicine Clinic’s handout on PRP injections.
The PRP injection
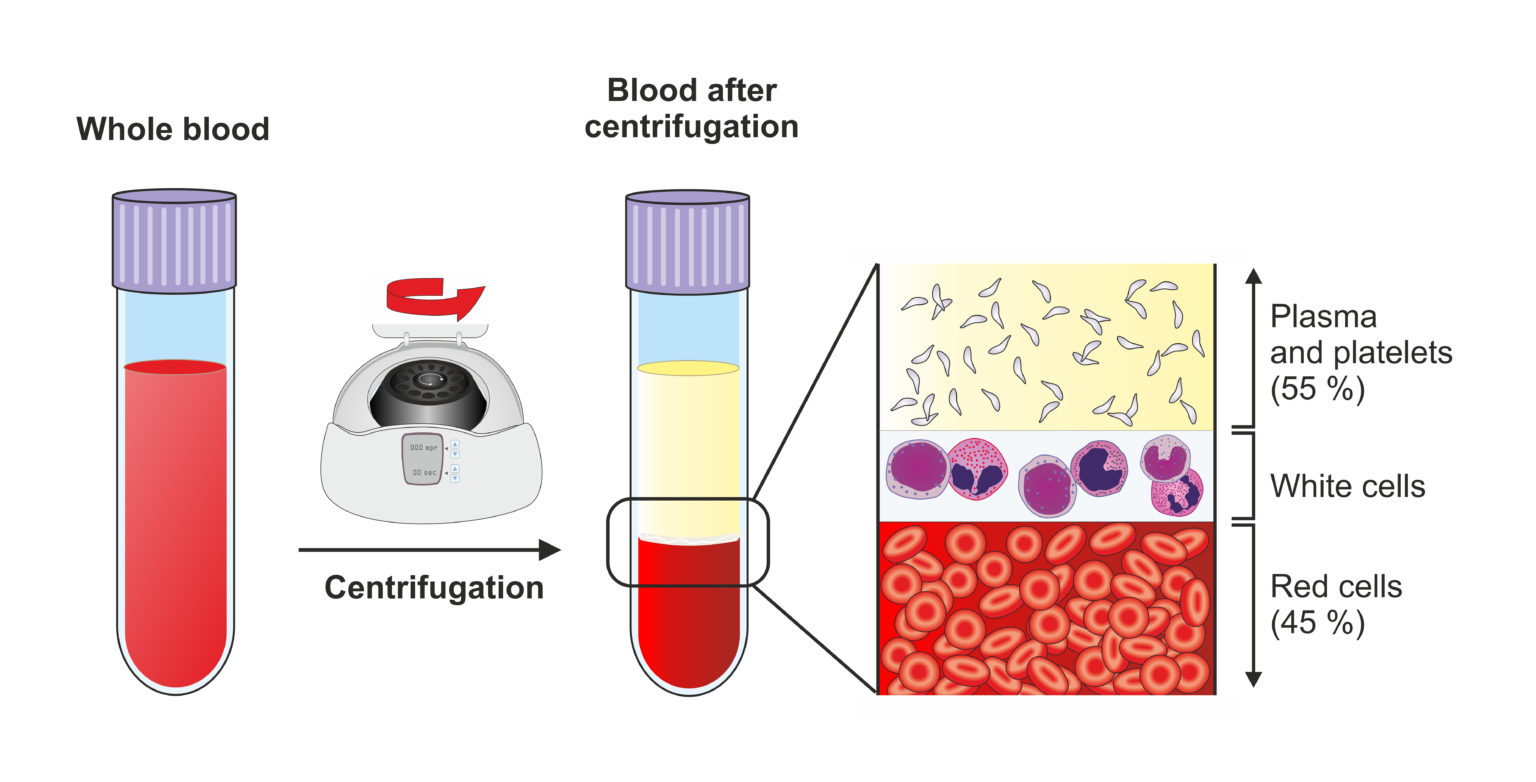
A small sample of the patient’s blood is collected, and an anticoagulant is added to stop the blood from clotting.
The sample is spun at high speed in a device called a centrifuge to separate the parts of the blood into layers: red blood cells, white blood cells (also called the ‘buffy coat’), and plasma.
The plasma and platelets (with or without WBCs depending on the commercial product used to prepare the PRP) are taken and injected into the injured joint. This is sometimes done using ultrasound guidance.
Recovery after PRP injection
Patients are asked to minimize activity and ice the area for 15-20 minutes every 2-4 hours for the first few days after the injection.
It is also recommended that patients limit major activity or strain of the treated area for at least a week, and sometimes up to three weeks, as patients who receive PRP that contains WBCs typically experience a temporary increase in pain.
It may take 6-8 weeks to assess the body’s response to the treatment.
Full recovery may take three to six months, with tendon injuries usually trending to longer recovery time.
— Learn more about injections offered at the Banff Sport Medicine Clinic —
What are the risks of PRP therapy?
Risks of PRP injection are quite limited because the preparation comes from the patient’s own blood.
As with any injection, uncommon risks include bleeding, bruising, nerve injury, and tissue damage.
What can PRP be used to treat?
The effects of PRP to treat specific injuries and conditions is still being actively investigated with mixed results. Here is some of what we know so far from a few clinical studies in patients.
| Name of condition/injury | Results |
|---|---|
| Mild to moderate knee and hip OA | A few studies have shown that PRP improved pain and function compared to treatment with pain medications such as acetaminophen and ibuprofen, and other injections such as hyaluronic acid |
| Tennis elbow (lateral epicondylitis) | Mixed results. Some studies show improved pain, and longer-lasting pain relief compared to anesthetic injections, while other studies show no difference |
| Golfer’s elbow (medial epicondylitis) | One study found patients reported faster pain reduction and reduced time to full range of motion when treated with PRP compared to surgery |
| Patellar tendinopathy | Mixed results. One study showed improved pain early in recovery relative to dry needling, but showed equal improvements after 26 weeks, while another study showed no difference |
| Plantar fasciitis | Two studies have so far shown PRP improves pain and function |
| Rotator cuff repair | Several studies have shown that PRP used in conjunction with arthroscopic surgery doesn’t appear to have benefit |
| Rotator cuff tendinitis | Mixed results. Some studies show a positive effect when using PRP compared to other non-surgical treatments, while other studies show no benefit |
| Achilles tendinopathy | Mixed results. Some studies show no different when using PRP, while other studies show Improved pain and function relative to a placebo (sham) injection |
| Achilles tendon repair | Mixed results. One study found that PRP used in addition to surgery was of no benefit, while another study found patients treated with PRP after surgery gained better range of motion. In addition, another study found no difference when using PRP versus a placebo (sham) injection to treat Achilles tendon ruptures. |
| Gluteal tendinopathy | One study showed favorable results compared to corticosteroid injection |
| Hamstring injury | Mixed results. Some studies have shown improved recovery time and reduced pain with PRP, while other studies have found no benefit |
In summary, PRP is a low-risk treatment that can be an effective therapy for some musculoskeletal injuries and conditions. However, further research is needed to prove the effectiveness of PRP treatment for specific injuries and conditions, and to determine the ideal preparation of PRP for each injury/condition.
Expert Contributor

Lisa Finestone, 4th Year MD Program, Faculty of Medicine and Dentistry, University of Alberta
References
Arumugam, S., Prakash, A., Janani, G., Vignesh, M., Anjanavannan, M. M., Perumal, S., & Alwar, T. (2021). Platelet-Rich Plasma (PRP) Injection in Sports Injuries. Indian Journal of Orthopaedics, 55(2), 484–491. https://doi-org.login.ezproxy.library.ualberta.ca/10.1007/s43465-020-00349-3
Bohlen, H.L., Schwartz, Z. E., Wu, V. J., et al. (2020). Platelet-Rich Plasma Is an Equal Alternative to Surgery in the Treatment of Type 1 Medial Epicondylitis. Orthopaedic Journal of Sports Medicine, 8(3). doi:10.1177/2325967120908952
John Hopkins Medicine. (n.d.). Platelet-Rich Plasma (PRP) Injections. Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/plateletrich-plasma-prp-treatment
Le, A., Enweze, L., DeBaun, M. R., & Dragoo, J. L. (2018). Current Clinical Recommendations for Use of Platelet-Rich Plasma. Current reviews in musculoskeletal medicine, 11(4), 624–634. https://doi.org/10.1007/s12178-018-9527-7
Lubkowska, A., Dolegowska, B., & Banfi, G. (2012). Growth factor content in PRP and their applicability in medicine. Journal of biological regulators and homeostatic agents, 26(2 Suppl 1), 3S–22S.
Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2013 Dec 23;(12):CD010071. doi: 10.1002/14651858.CD010071.pub2. Update in: Cochrane Database Syst Rev. 2014;(4):CD010071. PMID: 24363098.
O’Dowd A. Update on the Use of Platelet-Rich Plasma Injections in the Management of Musculoskeletal Injuries: A Systematic Review of Studies From 2014 to 2021. Orthop J Sports Med. 2022 Dec 9;10(12):23259671221140888. doi: 10.1177/23259671221140888.
Prodromos, C. C., Finkle, S., Prodromos, A. et al. Treatment of Rotator Cuff Tears with platelet rich plasma: a prospective study with 2 year follow‐up. BMC Musculoskelet Disord 22, 499 (2021). https://doi.org/10.1186/s12891-021-04288-4







