A tear of the medial meniscus posterior root is not just a meniscal tear: What should you know as a patient?
What are the menisci?
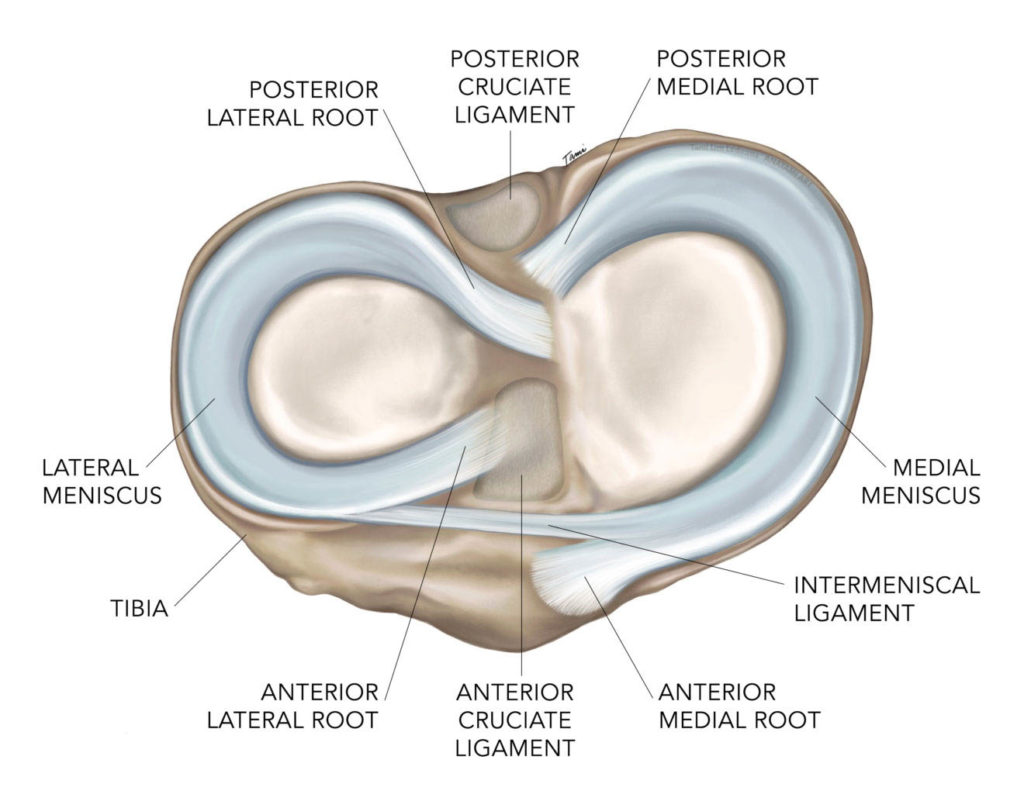
Menisci are soft-tissue C-shaped structures in the knee. There are two menisci in each knee: the medial meniscus (on the inside of the knee) and the lateral meniscus (on the outside of the knee). The menisci are located between the femur (thighbone) and the tibia (shinbone). Menisci are vital structures to the knee as they absorb shock and play a key role in knee stability.
A meniscus root is the attachment point of the meniscus to the tibia. Each meniscus is stabilized by an anterior (front) and a posterior (back) root, which act to anchor the menisci to the tibia.
What happens in the knee joint if you have a medial meniscus posterior root tear?
Research studies have shown that having a medial meniscus posterior root tear makes the medial meniscus non-functional. Essentially the same as having no meniscus.
In addition, studies have shown that the medial meniscus tends to extrude (bulge out of the weight-bearing zone) when the posterior root is torn. All of these factors combine to increase the chance of developing early osteoarthritis.
How do posterior root tears of the medial meniscus occur?
A medial meniscus posterior root tear is the most common amongst root tears. Almost 70% of these tears are chronic – which means they develop over time with no specific injury.
Sometimes, however, these tears can happen in conjunction with a knee ligament injury such as an ACL tear. Deep flexion and squatting are other common mechanisms that can injure the meniscal root.
Risk Factors
Risk factors for posterior root meniscal tears include:
- knee arthritis
- female sex
- increased age
- higher body mass index
- varus leg alignment (bow legged)
How can you tell the difference between a posterior root tear and a regular medial meniscus tear?
This is often very challenging, especially since most of these injuries are chronic and have a gradual onset.
In general, patients with standard meniscus tears will have joint-line tenderness (tenderness or pain in the knee joint where the femur and tibia meet) and symptoms of knee locking. However, patients with a meniscus root tear rarely report locking symptoms.
Acute (sudden) posterior root tears sometimes have a more abrupt onset, with a “pop” in the back of the knee, and a sudden increase in pain. Some people have even reported an almost immediate sense of a “bone on bone” feeling following an acute root tear injury.
How is this injury diagnosed?
- X-ray is used to eliminate other sources of pain, and may show signs of early arthritis like joint space narrowing which could signify meniscus extrusion. If the root tears at its bony insertion, a small fleck of bone may be seen in that location (this is called an avulsion fracture).
- MRI is the best imaging to diagnose a meniscal tear. However, only 73% of root tears will be visible on MRI.
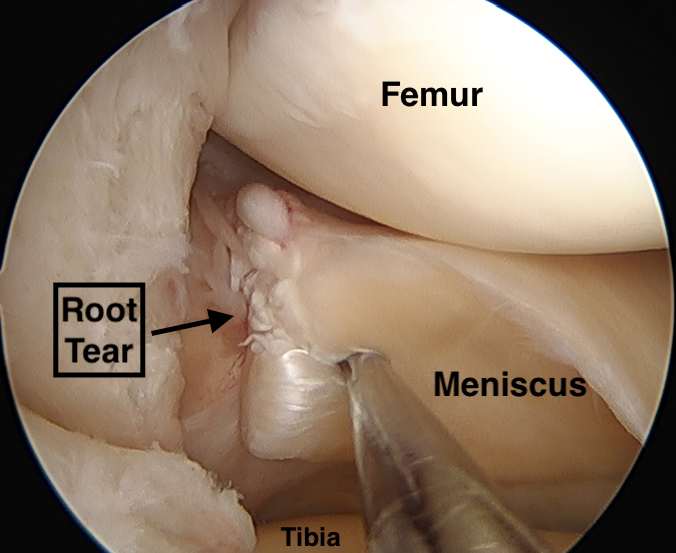
- Knee arthroscopy (surgery) is the gold standard to determine the presence of a medial meniscus posterior root tear.
- A lower limb alignment long-film radiograph may be necessary to determine if malalignment could have contributed to the root tear (i.e. varus, bow-legged alignment).
What is the treatment of a posterior root tear of the medial meniscus?
Non-surgical
Historically, these types of injuries have been treated conservatively, without surgery.
Non-surgical management includes physiotherapy to strengthen the surrounding muscles (the “dynamic” shock absorbers), medial unloader bracing, and anti-inflammatory medications. Lubricant joint injections (hyaluronic acid) can be helpful, particularly in patients with signs of osteoarthritis.
These kinds of treatment are often used in patients that aren’t suitable for surgical treatment. For example, older patients, those with significant comorbidities (such as severe cardiovascular or respiratory conditions ), those with advanced knee osteoarthritis, and those not willing to comply to a strict post-operative rehabilitation protocol.
Surgical
Surgical treatment options include arthroscopic surgery for meniscal debridement (a clean up), meniscal root repair, and lower limb realignment surgery (high tibial osteotomy).
The decision for when and what kind of surgery, is made on a case-by-case basis, taking into account all relevant patient factors. Some important considerations include: age, extent of osteoarthritis, leg alignment, BMI, and activity level. For example, surgical treatment is often used in patients that are young and physically active, without severe knee osteoarthritis, without severe varus malalignment of the legs, without a high BMI, and willing to comply with the post-operative rehabilitation.
After surgery, patients are typically asked to remain non-weight-bearing (also known as “feather” weight-bearing) for 4-6 weeks. Range of motion is restricted from 0 to 90 degrees of knee flexion for 6 weeks (sometimes in a hinged brace). Progressive weight-bearing, range of motion stretching, and strengthening resume at 6 weeks. By three months post-operative, most patients can return to low impact activities. Full recovery is expected around 6 months post-operative.
Biomechanical studies have demonstrated improved shock absorption and restoration of meniscal function following successful root repair, with most clinical studies showing improved patient quality of life (pain, function and activity scores) following surgery. In addition, some evidence supports a slower progression of osteoarthritis and reduced rates of knee replacement surgery in patients who have undergone a meniscal root repair. However, the healing potential and reduction of meniscal extrusion remains uncertain. Research is ongoing to help optimize surgical techniques and outcomes for patients with medial meniscus posterior root tears.
Contributing Expert
Dr. Philippe Beauchamp-Chalifour, MD, MSc, FRCSC, Orthopaedic Surgery, Université Laval
References
Allaire R, et al. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. Journal of Bone and Joint Surgery. 2008;90(9). 8
Allen CR, et al. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. Journal of Orthopaedic Research. 2000;18(1)
Bernard CD, et al. Medial Meniscus Posterior Root Tear Treatment: A Matched Cohort Comparison of Nonoperative Management, Partial Meniscectomy, and Repair. American Journal of Sports Medicine. 2020;48(1).
Bhatia S, et al. Meniscal root tears: Significance, diagnosis, and treatment. American Journal of Sports Medicine. 2014;42(12).
Choi CJ, et al. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy – Journal of Arthroscopic and Related Surgery. 2010;26(12).
Faucett SC, et al. Meniscus Root Repair vs Meniscectomy or Nonoperative Management to Prevent Knee Osteoarthritis After Medial Meniscus Root Tears: Clinical and Economic Effectiveness. American Journal of Sports Medicine. 2019;47(3).
Feucht MJ, et al. Arthroscopic Transtibial Pullout Repair for Posterior Medial Meniscus Root Tears: A Systematic Review of Clinical, Radiographic, and Second-Look Arthroscopic Results. Arthroscopy – Journal of Arthroscopic and Related Surgery. 2015;31(9).
Ishikawa H, et al. Arthroscopic Medial Meniscus Posterior Root Reconstruction and Pull-Out Repair Combined Technique for Root Tear of Medial Meniscus. Arthrosc Tech. 2022;11(2).
Jung YH, et al. All-inside repair for a root tear of the medial meniscus using a suture anchor. American Journal of Sports Medicine. 2012;40(6).
Krause WR, et al. Mechanical changes in the knee after meniscectomy. Journal of Bone and Joint Surgery – Series A. 1976;58(5).
Krych AJ, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(2).
Krych AJ, et al. Arthritis Progression on Serial MRIs Following Diagnosis of Medial Meniscal Posterior Horn Root Tear. Journal of Knee Surgery. 2018;31(7).
LaPrade RF, & Chahla J. Evidence-Based Management of Complex Knee Injuries. Elsevier; 2021.
LaPrade RF, et al. Posterior Meniscal Root Repairs: Outcomes of an Anatomic Transtibial Pull-Out Technique. American Journal of Sports Medicine. 2017;45(4).
Magee T. MR findings of meniscal extrusion correlated with arthroscopy. Journal of Magnetic Resonance Imaging. 2008;28(2).
Marzo JM. Medial Meniscus Posterior Horn Avulsion. Journal of the Academy of Orthopaedic Surgeons. 2009;17(5):276-283.
Marzo JM, & Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. American Journal of Sports Medicine. 2009;37(1).
Moon H-S, et al. Medial Meniscus Posterior Root Tear: How Far Have We Come and What Remains? Medicina. 2023; 59(7):1181.
Monson JK, & LaPrade RF. Posterior Medial Meniscus Root Tears: Clinical Implications, Surgical Management, and Post-operative Rehabilitation Considerations. Int J Sports Phys Ther. 2025 Jan 1;20(1):127-136.
Ozkoc G, et al. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surgery, Sports Traumatology, Arthroscopy. 2008;16(9).
Padalecki JR, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. American Journal of Sports Medicine. 2014;42(3).
Schnarkowski P, et al. Meniscal ossicle: Radiographic and MR imaging findings. Radiology. 1995;196(1).







