Postero-lateral corner instability of the knee: The basics
The knee’s stability relies on crucial connections between bones, muscles, ligaments, tendons, and fascia. Each structure is essential because, collectively, they enable us to move and carry out daily activities.
One important part of the knee is the postero-lateral corner (PLC).
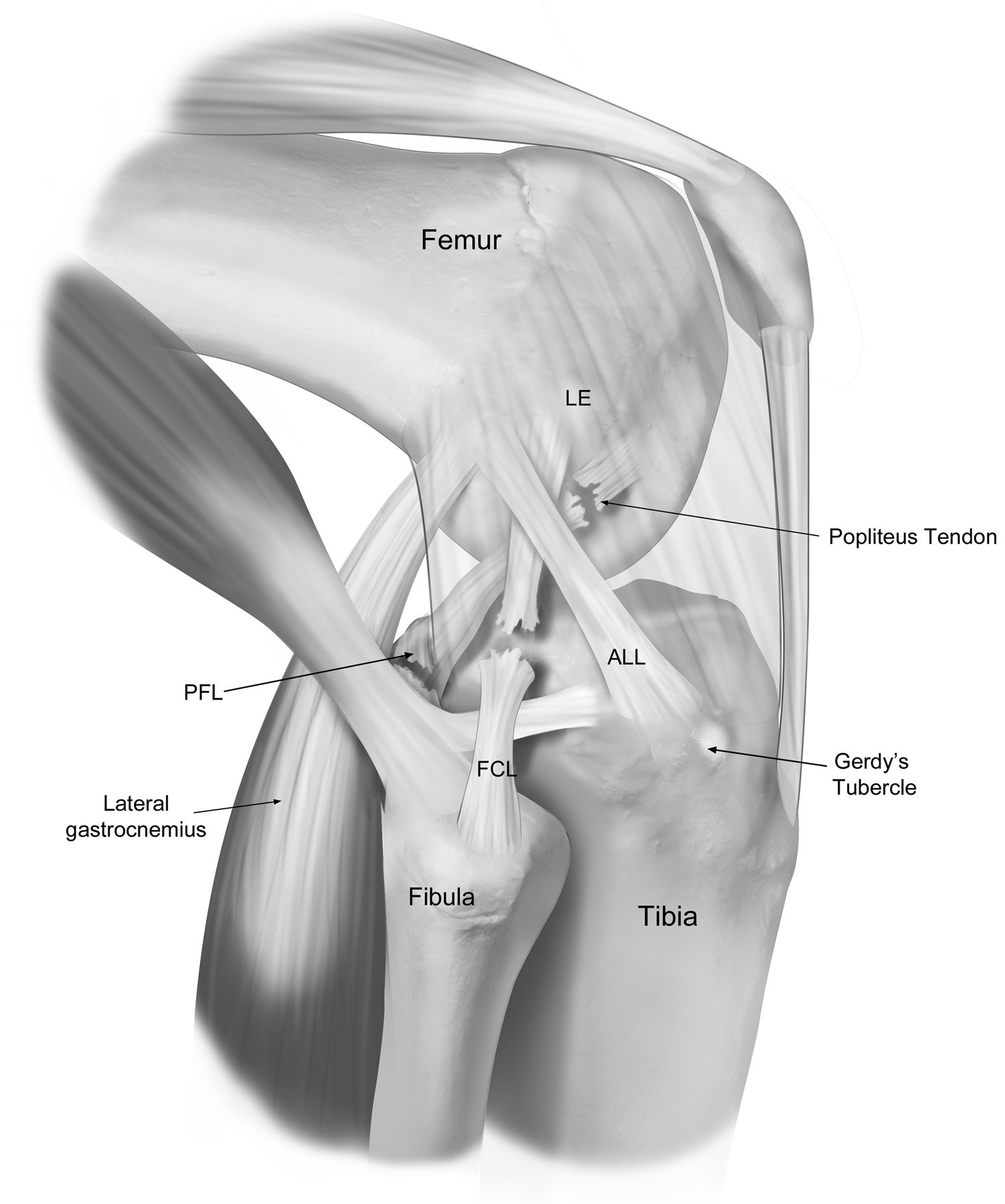
The PLC refers to a complex of structures on the back and outer side of the knee that help keep the knee stable. These structures include: the fibular (lateral) collateral ligament (FCL/LCL), the popliteus tendon (PLT), and the popliteofibular ligament (PFL).
These structures help to stabilize the knee, provide resistance to varus (outward bending) stress, and control the outward twisting of the lower leg.
Injury to the PLC
PLC injuries are most often caused by impact including direct varus stress (a force to the front-middle of your knee) or a non-contact hyperextension and external rotation injury. For example, you could injure your PLC playing a sport where someone makes a tackle and hits your knee causing it to twist, or your foot gets caught in the turf resulting in knee hyperextension.

In many cases, damage to the PLC is accompanied by injury to other parts of the knee, with research showing that PLC injury in isolation accounts for less than 30% of all PLC injuries.
These injuries are commonly linked with damage and tears to cruciate ligaments including the posterior cruciate ligament (PCL) and/or the anterior cruciate ligament (ACL).
Since PLC instability is frequently linked with injury elsewhere in the knee, it is important to consider how the PLC may be impacted when any injuries occur. These considerations become increasingly important during treatment since PLC damage can significantly impact the success of grafts used in reconstructing other cruciate ligaments, such as the ACL.
For example, an ACL reconstruction (ACL-R) graft may be at a higher risk of failure if the underlying PLC injury is not addressed. This is because the instability caused by a PLC injury places additional stress on the reconstructed ACL making it crucial to thoroughly evaluate and treat any PLC injuries to ensure the long-term success and stability of any ligament reconstruction.
Symptoms of PLC Injury
Symptoms for PLC injury and instability may vary but frequently reported symptoms include [3][6]:
- Minimal swelling and pain along the outside of the knee
- Side-to-side instability
- Increased difficulty walking on uneven ground or stairs
- difficulty twisting, turning and pivoting
- Foot drop (difficulty lifting the front of the foot upwards) with concurrent peroneal nerve injury
Diagnosis of PLC injury
Diagnosing PLC injuries can be challenging due to the complex anatomy of the knee that can result in this injury frequently being confused with other knee injuries (e.g. PCL and ACL injury).
PLC injuries can be diagnosed from thorough examination of the knee using special tests [5], checking active and passive range of motion, and performing a neurovascular exam [1][2]. Neurovascular exams are important to determine the function of the peroneal nerve which provides sensation to the front and sides of the leg as well as the top of the feet. Approximately 26% of PLC injuries result in damage to the peroneal nerve, which is why it is critical to examine its function post-injury.
Imaging techniques including MRI and X-ray can be used to help define the injury location/s and determine whether there are specific fractures and/or ligament damage. Additionally, information about the injury including direction of impact and subsequent symptoms can help to make a diagnosis.
Together, all of this helps to determine the severity of the instability and guide treatment decisions. There are 3 grades associated with PLC injuries which are classified by the Modified Hughston classification system:
- Grade I: Mild sprain with no major ligament damage.
- Grade II: Moderate injury with some ligament tearing.
- Grade III: Severe injury with complete ligament tearing.
Treatment of PLC Injury
Treatment for PLC injury can be either nonoperative or operative, depending on the severity of the injury.
When other injuries are present, treatment strategies are required to be more comprehensive as surgical timing, techniques, prioritization, and rehabilitation protocols may vary. As mentioned earlier, when reconstruction techniques are used for other cruciate ligament injuries including PCL and ACL damage, PLC stability must be examined to ensure success and stability in all parts of the knee.
- Nonoperative Treatment: Suitable for mild Grade I and isolated Grade II injuries (where no other knee ligament is injured). This typically involves using a hinged knee brace to immobilize the knee for about 4 weeks, followed by progressive functional rehabilitation and quadricep strengthening. Additionally, anti-inflammatory medications such as ibuprofen or naproxen can help reduce pain and swelling. In most cases, patients can return to sport 8 weeks after their injury.
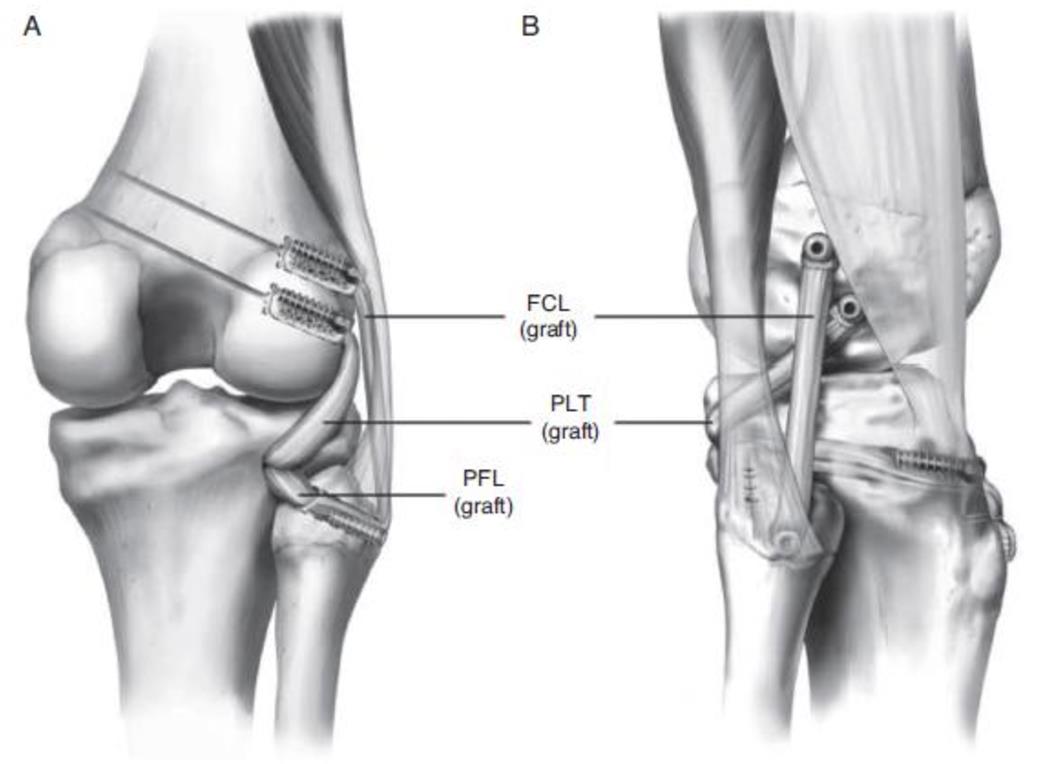
- Operative Treatment: Necessary for Grade III injuries. Surgical techniques aim to reconstruct key ligaments using tendon grafts to restore knee stability and function. When PLC injury is in conjunction with other ligamentous injuries, combined ligament reconstruction is often performed and multiple grafts may be used simultaneously. Grafts can be used to reconstruct damage in ligaments such as the FCL, PLT, and PFL. There are a few different reconstruction approaches and which method is used will depend on specific injury characteristics and surgical goals.
Rehabilitation after surgery involves using a hinged knee brace, avoiding weight-bearing for about 6 weeks, and following a tailored range of motion protocol. Anti-inflammatory medications (NSAIDs) such as ibuprofen or naproxen can help manage pain and swelling post-operation. Patients typically begin weight-bearing and light-strengthening activities around 6 weeks post-surgery and can return to sports within 6 to 9 months.
In summary, the ligaments and tendons forming the posterolateral corner of the knee are crucial for knee stability and function. Proper diagnosis and treatment of PLC injuries are essential to prevent long-term instability. With appropriate rehabilitation and care, individuals can regain knee stability and return to their active lifestyles.
Contributing Expert
Ellie Thompson, Life Sciences Honors Student, Queen’s University
References
Bassett, A. (2023, December 2). Posterolateral Corner Injury. Orthobullets. https://www.orthobullets.com/knee-and-sports/3012/posterolateral-corner-injury
Figueroa, F., Figueroa, D., Putnis, S., Guiloff, R., Caro, P., & Espregueira-Mendes, J. (2021a). Posterolateral Corner Knee Injuries: A Narrative Review. EFORT Open Reviews, 6(8), 676–685. https://doi.org/10.1302/2058-5241.6.200096
Hirschmann, M. T., & Müller, W. (2015). Complex function of the knee joint: The current understanding of the knee. Knee Surgery, Sports Traumatology, Arthroscopy, 23(10), 2780–2788. https://doi.org/10.1007/s00167-015-3619-3
Maheshwer, B., Drager, J., John, N. S., Williams, B. T., LaPrade, R. F., & Chahla, J. (2021). Incidence of intraoperative and postoperative complications after posterolateral corner reconstruction or repair: A systematic review of the current literature. The American Journal of Sports Medicine, 49(12), 3443–3452. https://doi.org/10.1177/0363546520981697
Maniar, Adit R. MBBS, MS; White, Alex E. MD; Musahl, Volker MD; Ranawat, Anil MD. Posterolateral Corner of the Knee: An Update on Current Evaluation and Management Strategies. Journal of the American Academy of Orthopaedic Surgeons 32(1):p e13-e23, January 1, 2024. | DOI: 10.5435/JAAOS-D-23-00278
Nahas, S., Patel, A., Hodgson, H., & Gupte, C. (2019). The posterolateral corner of the knee. Orthopaedics and Trauma, 33(2), 100–108. https://doi.org/10.1016/j.mporth.2019.01.003
Springer Nature Switzerland AG 2023 S. L. Sherman et al. (eds.), Knee Arthroscopy and Knee Preservation Surgery, https://doi.org/10.1007/978-3-030-82869-1_41-1







