Meniscal allograft transplantation: the basics
A meniscal allograft transplantation (MAT) is a type of surgery where a deficient or damaged meniscus from a patients’ knee is replaced with another meniscus of the same size from a deceased donor (cadaver).
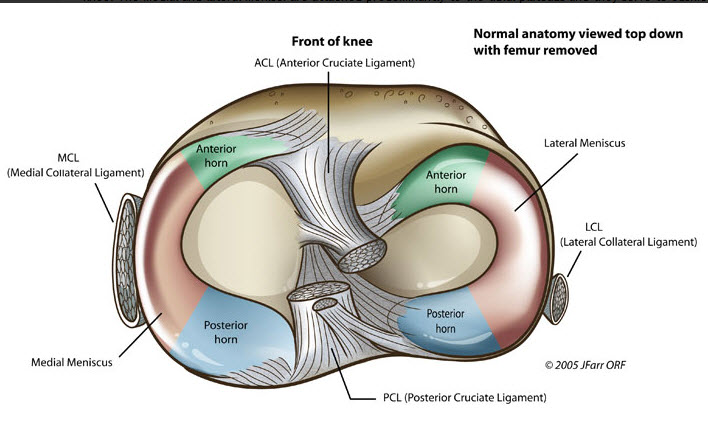
There are two menisci inside the knee joint as shown in the picture below: one on the inner side of knee, called the medial meniscus, and one on the outer side of knee, called the lateral meniscus. These C-shaped structures are made of a tough material called fibrocartilage and they attach to the top of the shin bone (tibia) and help to distribute weight-bearing load across and through the joint. The menisci also function as shock absorbers and have an important role in knee stability.
The meniscus is a type of cartilage inside the knee joint.


Traumatic meniscal injuries most commonly occur with sudden twisting of the knee on a planted foot. This can happen during activities that involve rapid changes of direction (cutting) and pivoting, such as soccer, basketball, and football.
Meniscal tears can also be found in combination with knee ligament injuries, the most common one being an anterior cruciate ligament (ACL) tear.
Many meniscal injuries can be treated with physiotherapy, but in some cases, a surgery may be needed. Sometimes the tear can be surgically repaired, but if there is a lot of damage, removal of the damaged part of the meniscus is required.
–Learn more about the basics of meniscal tears and how they’re treated here–
However, if part of, or all of, the meniscus is simply just removed, it will no longer function to distribute force, shock-absorb, or provide stability to the knee joint. Meniscal loss can also cause knee pain and instability, and ultimately may lead to early-onset osteoarthritis.
Therefore, replacing the damaged meniscus is necessary.
What is the aim of MAT?
The aim of an MAT is to restore normal meniscal function, reduce knee pain, and possibly slow down the progression of osteoarthritis.
Who is a good candidate for an MAT?
Selecting the correct patient is a KEY factor in having a favorable outcome.
An MAT can be helpful for young patients who have had most, or all, of their meniscus removed and are subsequently experiencing knee pain, swelling, and/or instability2.

Patients must also:
- Be less than 50 years old
- Have no (or very mild) knee osteoarthritis
- Have a body mass index less than 35
- Have normal knee alignment (i.e. not “knock-kneed” or “bow-legged”)
- Have a stable knee (intact knee ligaments)
Patients who do not have normal alignment or stable ligaments may need to undergo a realignment surgery (osteotomy) or ligament reconstruction before or at the same time as their MAT procedure.
At least 50% of MATs are performed in combination with these surgeries or with cartilage repair procedures3, 4.
— Learn more about osteotomy here —
What assessments happen before surgery?
In the office, your surgeon will obtain a thorough history of your symptoms, prior injuries, relevant surgeries, and activity level. You will undergo a physical exam to evaluate your walking (gait) and leg alignment, as well as your range of motion and ligament stability.
X-rays of your knees will be taken to identify bony injuries and to look for any evidence of degeneration (ie. osteoarthritis) in the joint. Additionally, full-length X-rays of your legs (hip to ankle) will be performed to measure your overall alignment. You may also need to have an MRI for images of your menisci, ligaments, and cartilage. Using your X-rays or your MRI, your surgeon will be able to measure the size of your meniscus so that a comparable replacement can be selected.
How is an MAT performed?
The meniscus allograft (transplant tissue) is taken from a deceased donor (cadaver), usually with the tibia bone still attached, and then sterilized by rapid deep freezing. When processed in this way, the tissue (called a fresh-frozen allograft) can be stored for up to 5 years.
Less commonly, fresh allografts are used; these grafts are not frozen, so the donor cells remain alive, but the tissue must be transplanted within 14 days.
Like other transplants, the donor allograft must be matched to the recipient. It is very important that the allograft (transplant) meniscus is similar in size to your meniscus; this helps the graft last longer5, 6.
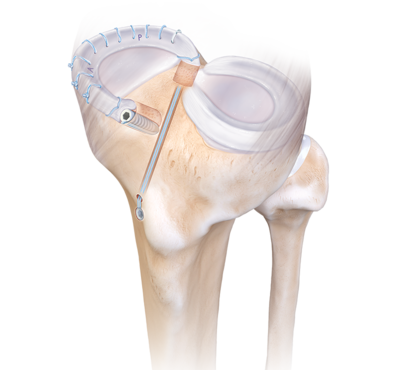
An MAT is usually performed with a small camera inside the knee joint (knee arthroscopy). First, the transplant site is prepared by trimming away most of your remaining meniscus. Then the allograft is inserted into your knee and fixed in place. The fixation can be performed in various ways, but those described below are the most common techniques used by the Orthopaedic Surgeons at the Banff Sport Medicine Clinic.
In a medial MAT (on the inner side of the knee), the attached bone on the meniscal allograft is shaped into two bone plugs, one on either end of the graft. These plugs are inserted into bone tunnels created in your tibia. Some long stitches (sutures) are attached to the bone plugs and brought out of the bone from the front of the tibia. Each set of sutures is tied over a small metal button on the surface of the bone; this button helps to secure the ends of the graft and prevents the sutures from being pulled back into the knee. Finally, the outer edge of the meniscus is secured in place with multiple sutures7.

In a lateral MAT (on the outer side of the knee), the allograft bone is shaped into a bridge connecting both ends of the meniscus graft. This bridge is inserted into a bony slot or trough created in your tibia. Again, the outer edge of the meniscus is stitched (sutured) down to hold it in place7.
What are the risks of this surgery?
The general risks of arthroscopic knee surgery can be found on the Banff Sport Medicine Surgery Information Resources webpage.
An MAT also has some special risks; because this procedure involves transferring tissue from a donor, there is a small possibility of disease transmission.
Fresh-frozen allografts (transplant tissues) undergo deep freezing and are soaked in an antibacterial solution, but further sterilization cannot be performed without weakening the graft tissue9. Because this process does not kill viruses, diseases such as HIV, Hepatitis B, and Hepatitis C may be transmitted.

However, tissue donors are carefully screened, so viral transmission is very rare, with the rate of HIV transmission ranging from 1 in 1 million to 1 in 8 million10, 11. Although bacterial diseases can also be transmitted, this risk is minimized by sterile allograft harvesting techniques and soaking of the tissue in antibacterial solutions. The risk of viral or bacterial transmission is higher with fresh allograft than with fresh-frozen allograft, but the overall risk of infection is still very low—much less than 0.1%12.
Another special risk of an MAT is the possibility for an immune reaction (rejection) to the allograft, although this is also extremely rare. This happens because your body recognizes a foreign tissue (the allograft) and tries to attack it. The risk of rejection may be higher in fresh allograft compared with fresh-frozen allograft13. It is still unknown how this immune response affects long term outcomes—while studies have not shown a clear association with symptoms or graft problems, this is still an area under investigation3, 14-16.
What should I expect after surgery?
For the first weeks after surgery, you will have some pain and swelling in your knee.
It is very important that you follow the post-operative protocol and recommendations provided by your surgeon as this will help you regain strength and range of motion, and avoid re-injury.
Initial rehabilitation focuses on protecting the new graft, regaining full extension of the knee, and recovering the quadriceps (thigh) muscle strength. All of these are important for achieving normal walking and recovery of knee function.
After the first few weeks, your rehabilitation will progress in a stepwise manner. Each phase has certain activity criteria that need to be met before moving to the next phase. Towards the later phases, the rehabilitation will become more tailored to your specific goals.
Even after the graft has healed, it is recommended that you continue to avoid contact pivoting sports as these may cause graft injury and failure.
What are the outcomes of an MAT?
Studies have shown promising short- and mid-term outcomes of MAT, with most patients experiencing improved pain and function after surgery.

These benefits are still found over 10 years after surgery13. Most patients (75%-77%) can return to sport or physical activity after surgery, with a lower proportion returning to their pre-injury level (48%-67%).
The average time to return to sport ranges from 9 to 12 months17, 18.
However, there is currently no long-term data regarding the return to high level, high-impact sport. These types of activities place the graft at risk of injury. For this reason, many surgeons recommend a return to low-impact sport only, such as cycling and swimming, to help preserve the graft.
One of the most common complications of an MAT is graft failure (the graft no longer functions properly). This might mean the graft has torn or has been extruded (pushed out) from the knee joint. If this happens, you may experience persistent knee pain.
Additionally, problems with the graft can lead to cartilage damage and “wear and tear” in the knee19. A second surgery, such as a total knee replacement or a revision MAT, may be required.
The risk of failure increases with time from surgery, with reoperation rates of 17.4% at 5 years, 37.4% at 10 years, and 40.9% at 15 years post-MAT20.
However, the majority of grafts are still functioning many years later—73.5% at 10 years and 60.3% at 15 years after MAT13.
Overall, research shows that, for the right patient, an MAT with or without associated procedures can be very beneficial for improving the symptoms of meniscal loss. MAT may also help younger patients delay (or even avoid) the need for a partial or full knee replacement.
Expert Contributor

Emily Chan, Orthopedic Surgery PGY-4, University of Saskatchewan
References
1. Baron SL, Jazrawi LM. Anatomy and Function. In: Strauss EJ, Jazrawi LM, eds. The Management of Meniscal Pathology: From Meniscectomy to Repair and Transplantation. Springer International Publishing; 2020:1-13.
2. Getgood A, LaPrade RF, Verdonk P, Gersoff W, Cole B, Spalding T. International Meniscus Reconstruction Experts Forum (IMREF) 2015 Consensus Statement on the Practice of Meniscal Allograft Transplantation. Am J Sports Med. May 2017;45(5):1195-1205. doi:10.1177/0363546516660064
3. Rosso F, Bisicchia S, Bonasia DE, Amendola A. Meniscal Allograft Transplantation: A Systematic Review. The American Journal of Sports Medicine. 2015/04/01 2014;43(4):998-1007. doi:10.1177/0363546514536021
4. De Bruycker M, Verdonk PCM, Verdonk RC. Meniscal allograft transplantation: a meta-analysis. Sicot j. 2017;3:33. doi:10.1051/sicotj/2017016
5. Stevenson C, Mahmoud A, Tudor F, Myers P. Meniscal allograft transplantation: undersizing grafts can lead to increased rates of clinical and mechanical failure. Knee Surgery, Sports Traumatology, Arthroscopy. 2019/06/01 2019;27(6):1900-1907. doi:10.1007/s00167-019-05398-2
6. Dienst M, Greis PE, Ellis BJ, Bachus KN, Burks RT. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med. Jan 2007;35(1):34-42. doi:10.1177/0363546506291404
7. Kopka M, Heard M, Getgood A. Meniscal Allograft Transplantation: Surgical Technique. In: Kim JG, ed. Knee Arthroscopy: An Up-to-Date Guide. Springer Singapore; 2021:275-293.
8. Gilat R, Verdonk P. Meniscus Deficiency and Meniscal Transplants. In: LaPrade RF, Chahla J, eds. Evidence-Based Management of Complex Knee Injuries. 2020:224-230:chap 19.
9. Suarez LS, Richmond JC. Overview of Procurement, Processing, and Sterilization of Soft Tissue Allografts for Sports Medicine. Sports Medicine and Arthroscopy Review. 2007;15(3):106-113. doi:10.1097/JSA.0b013e3180dca1fe
10. Buck B, Resnick L, Shah S, Malinin T. Human immunodeficiency virus cultured from bone. Implications for transplantation. Clinical orthopaedics and related research. 1990;(251):249-253.
11. McAllister DR, Joyce MJ, Mann BJ, Vangsness CT. Allograft Update: The Current Status of Tissue Regulation, Procurement, Processing, and Sterilization. The American Journal of Sports Medicine. 2007/12/01 2007;35(12):2148-2158. doi:10.1177/0363546507308936
12. Vangsness Jr CT, Dellamaggiora RD. Current safety sterilization and tissue banking issues for soft tissue allografts. Clinics in sports medicine. 2009;28(2):183-189.
13. Novaretti JV, Patel NK, Lian J, et al. Long-Term Survival Analysis and Outcomes of Meniscal Allograft Transplantation With Minimum 10-Year Follow-Up: A Systematic Review. Arthroscopy. Feb 2019;35(2):659-667. doi:10.1016/j.arthro.2018.08.031
14. Brophy RH, Matava MJ. Surgical options for meniscal replacement. J Am Acad Orthop Surg. May 2012;20(5):265-72. doi:10.5435/jaaos-20-05-265
15. Young J, Tudor F, Mahmoud A, Myers P. Meniscal transplantation: procedures, outcomes, and rehabilitation. Orthopedic research and reviews. 2017;9:35.
16. Rodeo SA, Seneviratne A, Suzuki K, Felker K, Wickiewicz TL, Warren RF. Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am. Aug 2000;82(8):1071-82. doi:10.2106/00004623-200008000-00002
17. Grassi A, Bailey JR, Filardo G, Samuelsson K, Zaffagnini S, Amendola A. Return to Sport Activity After Meniscal Allograft Transplantation: At What Level and at What Cost? A Systematic Review and Meta-analysis. Sports Health. 2019/03/01 2019;11(2):123-133. doi:10.1177/1941738118819723
18. Cvetanovich GL, Christian DR, Garcia GH, et al. Return to Sport and Patient Satisfaction After Meniscal Allograft Transplantation. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2020/09/01/ 2020;36(9):2456-2463. doi:https://doi.org/10.1016/j.arthro.2020.04.034
19. Cavendish PA, DiBartola AC, Everhart JS, Kuzma S, Kim WJ, Flanigan DC. Meniscal allograft transplantation: a review of indications, techniques, and outcomes. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. Nov 2020;28(11):3539-3550. doi:10.1007/s00167-020-06058-6
20. Vundelinckx B, Vanlauwe J, Bellemans J. Long-term Subjective, Clinical, and Radiographic Outcome Evaluation of Meniscal Allograft Transplantation in the Knee. The American Journal of Sports Medicine. 2014/07/01 2014;42(7):1592-1599. doi:10.1177/0363546514530092







