Influence of Patella Shape on Knee Instability
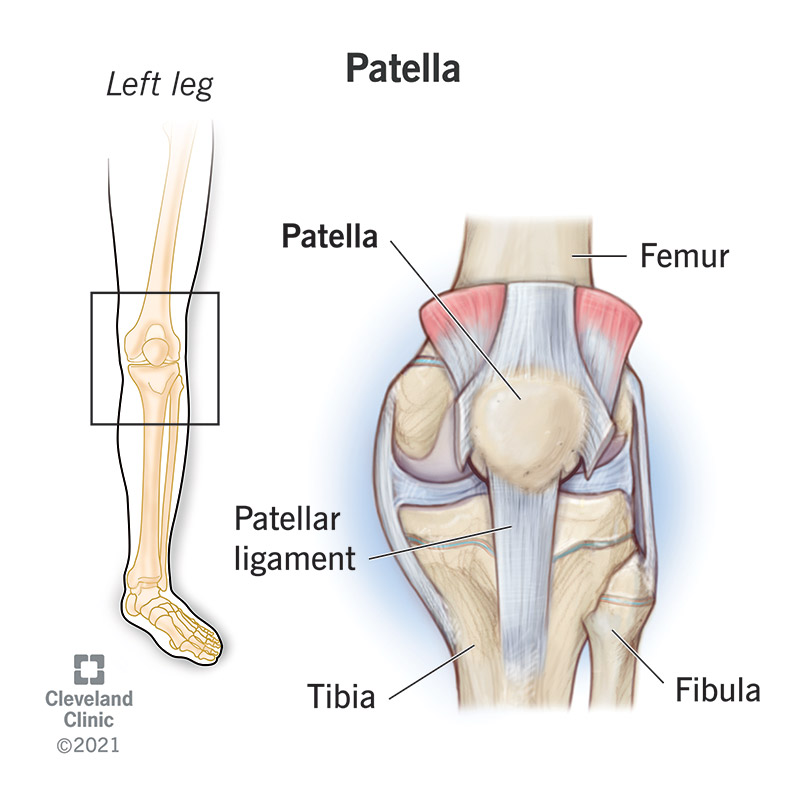
The patella (kneecap) is a small, triangular bone located at the front of your knee. It is a vital component in the knee joint, providing protection to the joint, and helping with knee extension when you straighten your leg (think walking, running, jumping).
Variations in Patella Shape
While most patellae share a similar shape, there are natural variations.
Some patellae are rounded, while others are flatter. Some exhibit a prominent ridge down the middle, while others are smoother.
These variations in shape can affect how the patella moves within its groove on the front of the knee. Some make it more likely for the patella to become unstable and slip out of place, a condition known as patellar instability.

One way to categorize these different shapes is the Wiberg classification, a system that examines the kneecap from above to see how symmetrical the inner and outer surfaces are. In this system, a higher classification number (or letter) indicates a greater degree of asymmetry between the surfaces.
For example, in a type I patella, the medial (the inside of the knee) and lateral (the outside of the knee) patellar facets (faces) are similar in size and are both concave. In type II, the medial patellar facet is shorter than the lateral facet, and both facets are concave. In the type III patella, the medial facet is much shorter than the lateral facet and is also convex
Causes of Patella Shape Variations
Patellar shape variations are influenced by a combination of factors:

- Genetics: Inherited traits play a significant role in determining the overall shape and structure of the patella. Certain genetic conditions such as nail patella syndrome, small patella syndrome, Meier-Gorlin syndrome, and genitopatellar syndrome, can lead to specific patellar shapes, like a smaller or more elongated patella.
- Development: The patella develops during childhood and adolescence, and any disruptions during this process can affect its final shape. This could be due to factors like abnormal growth patterns, trauma, or underlying skeletal conditions such as trochlear dysplasia (where the trochlear groove is shaped abnormally), patella alta (where the kneecap sits higher than normal), genu valgum (knock knees) and tibial torsion (where the shin bones twist inward).
- Muscle forces: The muscles surrounding the knee joint, particularly the quadriceps, exert forces on the patella that can influence its shape over time. Imbalances in muscle strength or abnormal tracking of the patella can lead to uneven stress distribution and contribute to shape variations.
- Joint alignment: The alignment of the knee joint, including the angle between the femur and tibia (Q angle), can affect how the patella tracks within the femoral groove. Misalignment can lead to abnormal wear patterns and contribute to changes in patellar shape.
- Injury and trauma: Fractures or dislocations of the patella can alter its shape, either due to the initial injury itself or the healing process. Scar tissue formation and remodeling of the bone can lead to variations in patellar morphology.
- Degenerative joint diseases: Degenerative joint diseases like osteoarthritis can cause wear and tear on the patella, leading to changes in its shape. The cartilage on the underside of the patella can erode, and bone spurs can develop, altering its overall morphology.
How Patella Shape Affects Stability
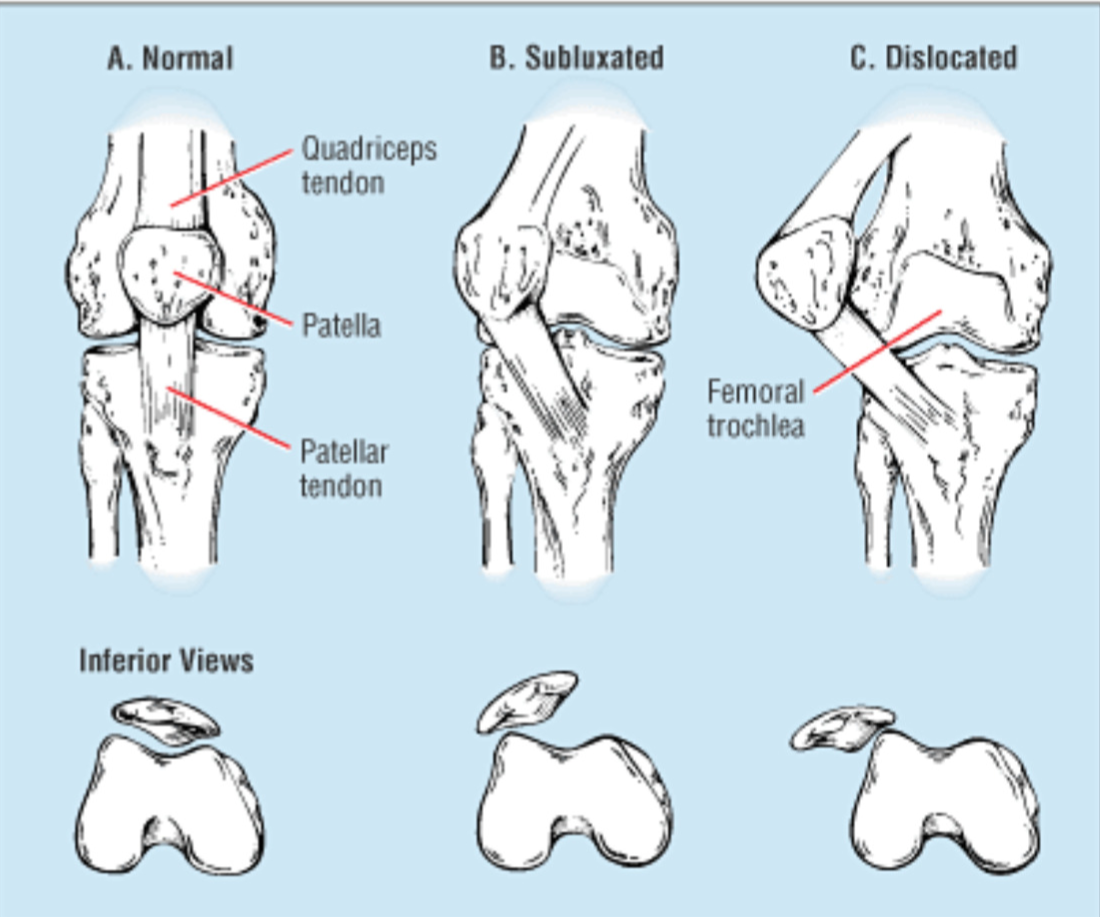
The shape of the patella directly impacts its ability to maintain stability within the knee joint. If the kneecap is unevenly shaped, it may not track smoothly within the trochlear groove, increasing its tendency to slip out of its proper position.
Additionally, differences in the size of the kneecap’s surfaces can create unbalanced forces, leading to uneven pressure distribution and an increased risk of dislocation. Therefore, whether partial (subluxation) or complete (dislocation), displacement of the kneecap can significantly contribute to knee joint instability.
Symptoms of patellar instability
Common symptoms of patellar instability include:
- Feeling of instability or giving way in the knee
- Popping or clicking sounds in the knee when you climb stairs or bend the knee
- Pain around the front of the knee (especially with activity)
- Swelling and Stiffness
- Limitations in function
Diagnosis and Treatment
Diagnosing patellar instability often involves a thorough physical examination, imaging studies (such as MRI), and assessing the patient’s symptoms and history of knee problems.
Treatment options vary depending on the severity of instability and may include:
- Physical Therapy: Exercises to strengthen the quadriceps and improve patellar tracking can be highly beneficial.
- Bracing: A knee brace can offer extra support for the patella and help maintain its position.
- Surgical Intervention: In some cases, surgery may be necessary to correct the underlying cause of instability. Examples of surgical treatments include a medial patellofemoral ligament reconstruction, or a tibial tubercle osteotomy.
Understanding the influence of patella shape on knee instability is crucial for both patients and healthcare providers. By recognizing the potential impact of patella shape variations, early intervention and appropriate management strategies can be implemented to prevent further complications and improve overall knee function.
Contributing Expert

Maria Mohorea, Health Science Honors Student, McMaster University
References
- Bongers, E. M., van Kampen, A., van Bokhoven, H., & Knoers, N. V. (2005). Human syndromes with congenital patellar anomalies and the underlying gene defects. Clinical genetics, 68(4), 302–319. https://doi.org/10.1111/j.1399-0004.2005.00508.x
- Colvin, A. C., & West, R. V. (2008). Patellar instability. Sports medicine and arthroscopy review, 16(4), 232-238.
- Loudon, J. K. (2016). BIOMECHANICS AND PATHOMECHANICS OF THE PATELLOFEMORAL JOINT. International journal of sports physical therapy, 11(6), 820–830.
- Noyes, F. R. (2009). Noyes’ Knee Disorders: Surgery, rehabilitation, clinical outcomes e-book. Saunders.
- Panni, A. S., Cerciello, S., Maffulli, N., Di Cesare, M., Servien, E., & Neyret, P. (2011). Patellar shape can be a predisposing factor in patellar instability. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA, 19(4), 663–670. https://doi.org/10.1007/s00167-010-1329-4
- Parikh, S. N., Veerkamp, M., Redler, L. H., Schlechter, J., Williams, B. A., Yaniv, M., Friel, N., Perea, S. H., Shannon, S. R., & Green, D. W. (2022). Patellar Instability in Young Athletes. Clinics in sports medicine, 41(4), 627–651. https://doi.org/10.1016/j.csm.2022.05.005
- Wiberg, G. (1941). Roentgenographs and anatomic studies on the femoropatellar joint: With special reference to chondromalacia patellae. Acta Orthopaedica Scandinavica, 12(1–4), 319–410. https://doi.org/10.3109/17453674108988818
- Wolfe, S., Varacallo, M., Thomas, J.D., Carroll, J.J., & Kahwaji, C.I. (2023). Patellar Instability. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482427/